Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Anatomy of Male Genitalia
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Anatomy of the Oesophagus |Anatomy of the Diaphragm |Anatomy of Large Bowel |Anatomy of Small Bowel |Anatomy of the Biliary system |Anatomy of the Eye |Anatomy of the Larynx |Anatomy of the Ear |Anatomy of the Pharynx |Anatomy of the Nose |Anatomy of Male Genitalia |Anatomy of Breast |Anatomy of the Stomach |Anatomy of the Rectum |Anatomy of the Spleen |Anatomy of the Liver
Introduction
The male genital system is an essential component of the reproductive system. It not only produces, matures, and transports sperm but also synthesizes and secretes testosterone. The anatomy can be broadly divided into external and internal structures, each with distinct functions and complex interrelationships.
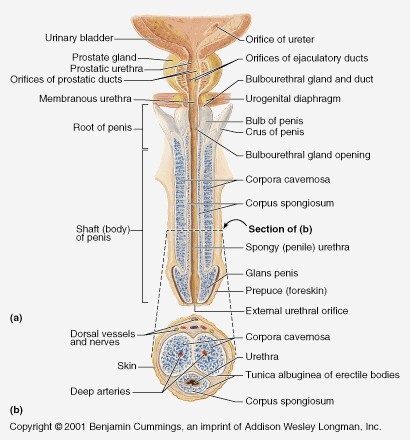
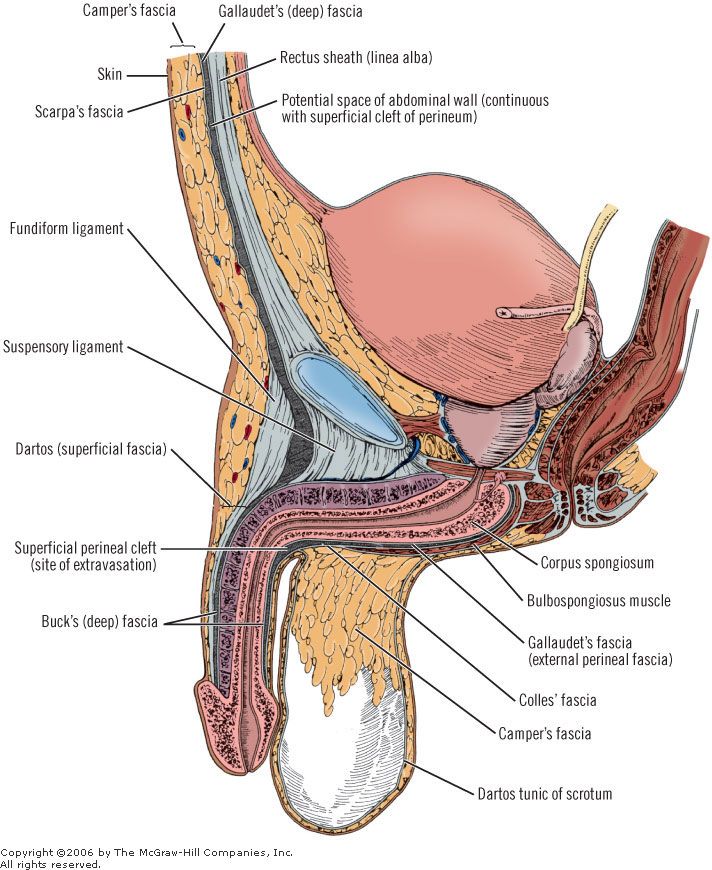
External Genitalia
- Penis:
- Glans Penis: The conical, highly sensitive tip, typically covered by the foreskin in uncircumcised males.
- Corpus Cavernosum: Two parallel erectile tissues that run along the dorsal side; these become engorged with blood during sexual arousal to produce an erection.
- Corpus Spongiosum: A single erectile tissue that surrounds the urethra, preventing its compression during erection and forming the expanded tip (glans).
- Frenulum: A V-shaped band of tissue on the ventral side of the penis that connects the glans to the shaft and plays a role in sexual sensitivity.
- Scrotum:
- A pendulous sac of skin, connective tissue, and smooth muscle (dartos) that suspends and protects the testes.
- The scrotum’s thin, highly vascularized skin and underlying muscle help regulate testicular temperature, which is critical for optimal sperm production.
- A median raphe divides the scrotum into two compartments, each containing one testis.
Internal Genitalia
- Testes:
- Paired oval organs located within the scrotum that produce sperm (spermatogenesis) and secrete testosterone.
- Each testis is surrounded by a tough fibrous capsule (tunica albuginea) and contains seminiferous tubules where sperm production occurs.
- Epididymis:
- A coiled, crescent-shaped tube situated along the posterior surface of each testis that serves as the site for sperm maturation and storage.
- Vas Deferens (Ductus Deferens):
- A long, muscular tube that transports mature sperm from the epididymis to the ejaculatory ducts during ejaculation.
- Ejaculatory Ducts:
- Short ducts formed by the union of the vas deferens and the duct of the seminal vesicle; they empty into the prostatic urethra.
- Accessory Glands:
- Seminal Vesicles: Glands that secrete a viscous, fructose-rich fluid, which provides energy and a medium for sperm transport.
- Prostate Gland: A walnut-sized gland that produces a milky alkaline fluid; this fluid enhances sperm motility and longevity while neutralizing the acidic environment of the female reproductive tract.
- Bulbourethral (Cowper's) Glands: Small glands that secrete a clear, mucous fluid before ejaculation to lubricate the urethra and neutralize traces of acidic urine.
Blood Supply, Innervation, and Lymphatic Drainage
- Blood Supply:
- The internal pudendal artery, a branch of the internal iliac artery, is the primary source of blood. Its branches—such as the deep and dorsal penile arteries—supply the penis and scrotum.
- Nerve Supply:
- The pudendal nerve (S2–S4) provides somatic sensory and motor innervation to the external genitalia.
- Autonomic innervation, through sympathetic and parasympathetic fibers, regulates vascular changes crucial for erection and ejaculation.
- Lymphatic Drainage:
- Lymph from the penis and scrotum primarily drains into the superficial inguinal lymph nodes, while deeper structures like the testes drain into the para-aortic lymph nodes.
Embryology and Development
The male genitalia develop from the embryonic genital tubercle, urogenital folds, and labioscrotal swellings. Under the influence of androgens (testosterone and dihydrotestosterone), these structures differentiate into the penis and scrotum. The testes originate in the abdominal cavity and descend into the scrotum during fetal development—a process essential for maintaining a temperature conducive to spermatogenesis.
Clinical Correlations
- Congenital Anomalies:
- Hypospadias: A condition in which the urethral opening is abnormally located on the underside of the penis.
- Cryptorchidism: Failure of one or both testes to descend into the scrotum, which may increase the risk of infertility and testicular cancer.
- Infections and Inflammations:
- Epididymitis, orchitis, and prostatitis are common conditions affecting various parts of the male genital tract.
- Cancers:
- Testicular, prostate, and penile cancers are significant clinical concerns with established screening and treatment protocols.
Conclusion
The detailed anatomy of the male genital system encompasses a complex interplay between external structures (penis and scrotum) and internal organs (testes, accessory glands, and ductal systems). Understanding the precise structure, blood supply, innervation, and lymphatic drainage is crucial for diagnosing and managing clinical conditions ranging from congenital anomalies and infections to cancers.