Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Graves Disease (Thyrotoxicosis)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Thyrotoxicosis and Hyperthyroidism |Thyroid Storm - Thyrotoxic crisis |Graves' Disease (Thyrotoxicosis) |Amiodarone and Thyroid disease |Thyroid Surgery (Thyroidectomy) |Hypothyroidism |Hashimoto's thyroiditis |DeQuervain's thyroiditis |Subacute Thyroiditis |Thyroid nodule |Congenital Hypothyroidism |Thyroid Function Tests and antibodies |Post partum thyroiditis |Sick Euthyroid Syndrome |Thyroid Exam (OSCE) |Thyroid Gland anatomy and Physiology |Thyroid Cancer
⚠️ Smokers with Graves' Disease have a much higher risk of developing thyroid eye disease (TED). Smoking cessation is essential to reduce complications and improve treatment outcomes.
📖 About
- Autoimmune disease: Graves’ disease is the commonest cause of hyperthyroidism (60–80% of cases).
- It is the leading cause of thyrotoxicosis in the UK.
🔎 Risk Factors
- Gender: Women >> Men (≈10:1 ratio).
- Age: Typically 30–50 years.
- Postpartum: Increased risk after childbirth.
- Smoking: Strongest risk factor for thyroid eye disease.
🧬 Aetiology
- Genetic: Linked to HLA-B8, DR3.
- TSH Receptor Antibodies (TRAb): Found in 80–90%; stimulate follicular hyperplasia and cross placenta.
- Thyroid Peroxidase (TPO) antibodies: Present in ~80% of cases.
- Eye disease: Fibroblast activation + glycosaminoglycan deposition → orbital swelling & proptosis.
🩺 Clinical Presentation
- Symptoms: Weight loss, anxiety, palpitations, tachycardia, heat intolerance.
- Elderly: May present with apathetic thyrotoxicosis.
- Exam: Diffuse goitre with thrill/bruit from ↑ vascularity.
🌟 Graves’ Disease–Specific Signs
- Eye disease (TED): In ~40%. Includes lid lag, lid retraction, proptosis, diplopia, corneal ulceration.
- Pretibial Myxoedema: Pink–orange shin plaques (~5%).
- Acropachy: Thyroid-related clubbing with onycholysis (rare).
🔬 Investigations
- Thyroid hormones: ↑ T4/T3, suppressed TSH (<0.05 mIU/L).
- TRAb: Specific for Graves’ disease.
- Radionuclide scan: Diffuse uptake (vs nodular in toxic adenoma).
🧾 Differentials
- Toxic multinodular goitre
- Toxic adenoma
- Excess exogenous thyroxine (iatrogenic)
⚕️ Management
- Symptom control: Beta-blockers (e.g. propranolol).
- Antithyroid drugs: Carbimazole (20–40 mg) or Propylthiouracil.
- Radioiodine therapy: Avoid in active eye disease (worsens TED, esp. in smokers).
- Surgery: Subtotal thyroidectomy for severe/refractory disease.
- Complication prevention: Anticoagulate in atrial fibrillation.
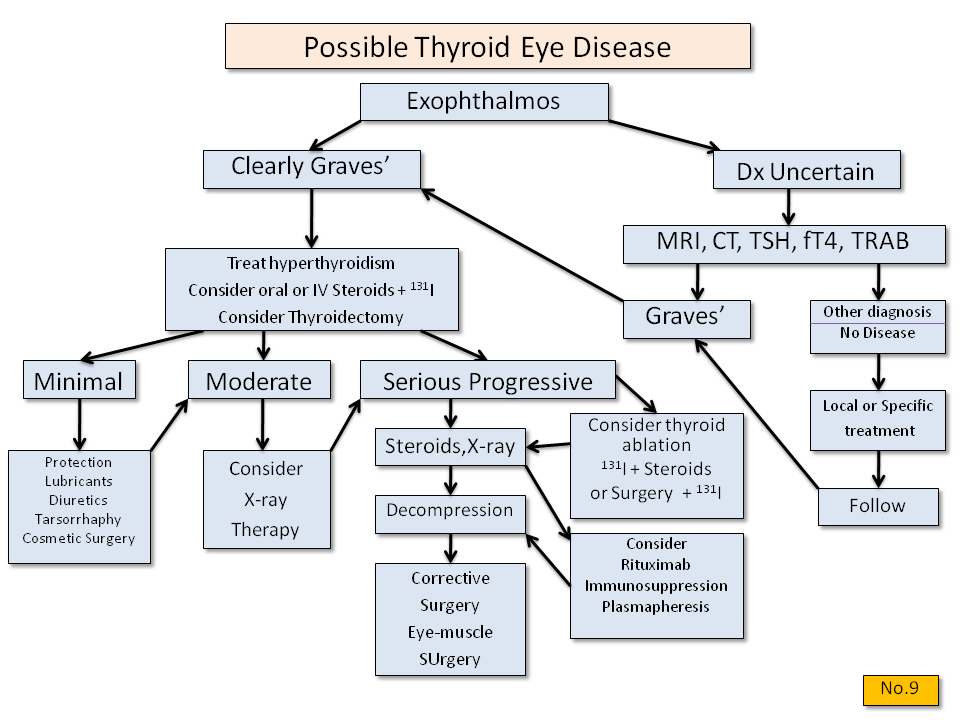
👁️ Thyroid Eye Disease Management
- First muscle involved: Inferior rectus → restricted upgaze.
- Stop smoking: Absolutely essential.
- Ophthalmology referral: Monitor acuity, intraocular pressure, and optic nerve health.
- Conservative: Lubricant drops, patching, head elevation.
- Medical: Steroids (e.g. prednisolone 60 mg), ciclosporin, plasma exchange, rituximab.
- Advanced: Orbital radiotherapy or decompression in sight-threatening disease.
💡 Key Exam Tip: In a hyperthyroid patient who smokes, always enquire about eye symptoms. Active TED is an important contraindication to radioiodine treatment.