Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Horner's syndrome
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🦉 Horner’s Syndrome is caused by the loss of sympathetic nerve supply to the face and eye. It classically presents with ptosis, miosis, anhidrosis, and apparent enophthalmos. ⚠️ Important causes to exclude: lung apex malignancy (Pancoast tumour), carotid artery dissection, and lateral medullary infarct.
📍 Aetiology
- The sympathetic pathway originates in the hypothalamus, descends through the brainstem, exits at C8/T1, travels with the carotid artery, and finally enters the eye.
- Lesions along this 3-neuron pathway produce Horner’s syndrome.
🧠 Causes (By Neuron Level)
- First-order (Central): Brainstem and cervical cord lesions
- Stroke (especially lateral medullary syndrome).
- Tumours, demyelination (e.g., MS).
- Syringomyelia, trauma.
- Second-order (Preganglionic): Apex of lung / chest outlet
- Pancoast tumour (lung apex squamous carcinoma).
- Thoracic trauma or post-surgical damage.
- Schwannoma.
- Third-order (Postganglionic): Neck / carotid artery to the eye
- Carotid artery dissection or aneurysm.
- Base of skull tumours or infections.
- Cluster headaches / migraines.
- Birth trauma in children.
📊 Anatomy of Autonomic Supply
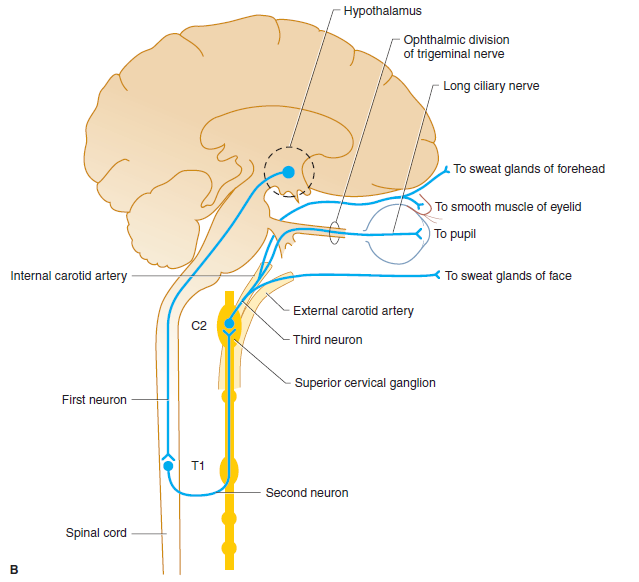
This 3-neuron oculosympathetic pathway runs: Hypothalamus → Spinal cord (C8–T1) → Superior cervical ganglion → Eye (pupil dilator, eyelid smooth muscle, facial sweat glands).
🩺 Clinical Features
- 👁️ Ptosis: Drooping of upper eyelid (loss of sympathetic innervation to Müller’s muscle).
- 🎯 Miosis: Constricted pupil that reacts normally to light.
- 💧 Anhidrosis: Reduced sweating on affected side (distribution depends on lesion level).
- ⚡ Apparent enophthalmos: Sunken eye appearance.
- Additional: Conjunctival injection; cough and cachexia if lung cancer-related.
📸 Case Studies
- Left Pancoast Tumour: Horner’s with ptosis from apical lung cancer.

- Idiopathic Horner’s: Left-sided, cause unknown.

- Classic Clinical Signs: Ptosis + miosis + anhidrosis.

🧪 Investigations
- Bloods: FBC, U&E; calcium or sodium derangements may suggest paraneoplastic lung cancer.
- Imaging:
- MRI brainstem for stroke.
- MRA neck for carotid dissection.
- CT chest for apical lung tumour (Pancoast).
- Pharmacological Testing:
- 1% cocaine drops: failure of pupil dilation confirms Horner’s.
- Apraclonidine drops may also be used (denervation supersensitivity → pupil dilates).
🩹 Management
- 🎯 Treat the underlying cause:
- Surgery / radiotherapy for lung cancer.
- Anticoagulation or stenting for carotid dissection.
- Stroke management if central cause.
- 👁️ Symptom management: Usually benign, but underlying pathology must never be missed.
💡 Clinical Pearls
- Think “Ptosis + Miosis + Anhidrosis = Horner’s until proven otherwise”.
- Always exclude 🚬 Pancoast tumour in a smoker with Horner’s + arm/shoulder pain.
- 🚑 Carotid dissection is a stroke emergency: look for ipsilateral head/neck pain + Horner’s.
Cases — Horner’s Syndrome
- Case 1 — Apical Lung Tumour (First-Order Neuron) 🫁: A 62-year-old man with a 40 pack-year smoking history presents with right-sided shoulder pain radiating to the arm. Exam: mild right ptosis, miosis, and anhidrosis. CXR shows a right apical mass. Diagnosis: Horner’s syndrome due to Pancoast tumour invading sympathetic chain. Management: Oncology referral; CT chest; biopsy for staging.
- Case 2 — Carotid Artery Dissection (Second-Order Neuron) ⚡: A 45-year-old man presents with sudden neck pain and headache after minor trauma. Exam: left ptosis and miosis without anhidrosis; no extraocular palsy. MRI angiography: left internal carotid artery dissection. Diagnosis: Painful Horner’s syndrome due to carotid dissection. Management: Urgent vascular input; anticoagulation/antiplatelets; stroke prevention.
- Case 3 — Cluster Headache (Third-Order Neuron) 💥: A 38-year-old man has recurrent severe left periorbital headaches lasting 1 hour, associated with ipsilateral lacrimation and nasal congestion. Exam during attack: mild ptosis and miosis on the left. Diagnosis: Horner’s syndrome associated with cluster headache. Management: High-flow oxygen, subcutaneous sumatriptan for acute attack; verapamil for prevention.
- Case 4 — Stroke-Related Horner’s 🧠: A 59-year-old man with vascular risk factors presents with acute vertigo, dysphagia, hoarseness, and loss of pain/temperature sensation on the right side of his face and left body. Exam: right-sided ptosis and miosis. MRI brain: infarct in right lateral medulla (posterior inferior cerebellar artery territory). Diagnosis: Horner’s syndrome secondary to lateral medullary (Wallenberg’s) syndrome. Management: Stroke care (antiplatelet therapy, risk factor modification, swallow assessment, rehab); supportive for Horner’s.
Teaching Commentary 🧠
Lateral medullary syndrome = classic brainstem stroke syndrome (PICA or vertebral artery occlusion). Key features: - Ipsilateral: facial pain/temperature loss (trigeminal nucleus), Horner’s syndrome (sympathetic tract), ataxia (cerebellar peduncle), palate weakness (nucleus ambiguus → dysphagia/hoarseness). - Contralateral: body pain/temperature loss (spinothalamic tract). Mnemonic: “Don’t PICA horse (hoarseness) that can’t eat (dysphagia)”. Management: same as ischaemic stroke (antiplatelets, risk factor control, swallow therapy). Prognosis depends on severity of bulbar dysfunction.