Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Diabetes Insipidus
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🧪 Vasopressin (antidiuretic hormone, ADH; arginine vasopressin, AVP) is a nonapeptide synthesised in the hypothalamus and stored in the posterior pituitary. 💧 It is the key regulator of water reabsorption in the distal nephron. 📈 A rise in plasma osmolality of as little as 1% (threshold ~280–285 mOsm/kg H₂O) triggers AVP release → water retention + concentrated urine.
📖 About
- Produced in the supraoptic & paraventricular nuclei of the hypothalamus, stored in the posterior pituitary.
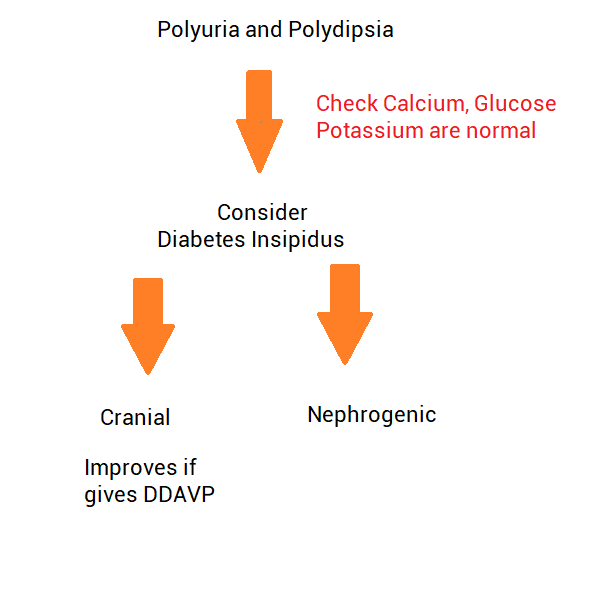
- Diabetes Insipidus (DI) = failure of AVP secretion or action → inability to concentrate urine → polyuria, polydipsia, hypernatraemia risk.
- 👉 Cranial DI: Impaired secretion.
👉 Nephrogenic DI: Kidneys unresponsive. - Severe DI: urine output can exceed 10–12 L/day.
⚙️ Physiology
- AVP release is controlled by plasma osmolality & blood volume/pressure.
- Acts via V2 receptors on collecting duct principal cells.
- Activates cAMP–PKA pathway → insertion of aquaporin-2 channels.
- Effect: ↑ water reabsorption, ↓ urine output, concentrated urine.
🧬 Aetiology
- Loss of AVP action → uncontrolled free water loss.
- If water intake inadequate → ⚠️ rapid dehydration & hypernatraemia.
- Note: >80–90% hypothalamic neuron loss needed before symptoms appear.
🧠 Cranial (Central) DI – Causes
- Idiopathic (most common in adults).
- Trauma, neurosurgery, craniopharyngioma.
- Sarcoidosis, TB, histiocytosis X.
- Meningitis, encephalitis, subarachnoid haemorrhage.
- Familial (rare, AD inheritance).
- Syndromic (e.g. DIDMOAD: DI, DM, optic atrophy, deafness).
🧩 Nephrogenic DI – Causes
- 💊 Drugs: Lithium, demeclocycline.
- ⚡ Electrolytes: Hypercalcaemia, hypokalaemia.
- CKD: Pyelonephritis, obstruction, amyloidosis, PKD.
- Inherited mutations: V2 receptor or aquaporin-2 defects.
- Systemic: Sickle cell disease, sarcoidosis.
📋 Clinical Features
- 💧 Polyuria: large volumes of dilute urine.
- 🚰 Polydipsia, intense thirst.
- ⚠️ Hypernatraemia if fluid intake inadequate → confusion, seizures, coma.
- ↑ VTE risk from haemoconcentration.
🔬 Investigations
- 🩺 Bloods: U&E (↑ Na⁺), ↑ plasma osmolality.
- 🧪 Urine: low osmolality despite high volume.
- 💡 Water deprivation test: confirms DI.
– Central DI: urine concentrates after desmopressin.
– Nephrogenic DI: no response to desmopressin. - Consider MRI brain (pituitary/hypothalamus).
🔎 Differential of Polyuria
- Diabetes mellitus (osmotic diuresis).
- Hypercalcaemia.
- Diuretics.
- Psychogenic polydipsia (excessive fluid intake).
- CKD.
- Post-obstructive diuresis.
💊 Management
- Cranial DI: Desmopressin (DDAVP) – intranasal, oral, or injection. ⚠️ Monitor for hyponatraemia.
- Nephrogenic DI: Low-salt diet, thiazides ± amiloride. NSAIDs (indomethacin) can ↓ urine output.
- Lithium-induced DI: Amiloride (blocks lithium uptake in collecting duct). Stop lithium if possible.
- General: Careful correction of hypernatraemia – avoid rapid shifts (risk of cerebral oedema).
📚 Teaching Pearls
💡 Exam buzzwords: Polyuria + hypernatraemia + low urine osmolality. 💡 Always distinguish from diabetes mellitus (check urine glucose). 💡 Water deprivation + desmopressin test = gold standard. 💡 In psychiatry patients with polydipsia, always consider psychogenic vs DI.
📚 References
Cases — Diabetes Insipidus (DI)
- Case 1 — Central DI after Pituitary Surgery 🧠: A 45-year-old woman develops sudden-onset polyuria (8 L/day) and polydipsia following transsphenoidal surgery for a pituitary macroadenoma. Urine: very dilute (osmolality 80 mOsm/kg). Plasma sodium: 152 mmol/L. Diagnosis: Central diabetes insipidus (loss of ADH secretion). Management: Desmopressin (DDAVP); fluid replacement; monitor electrolytes closely.
- Case 2 — Nephrogenic DI from Lithium 💊: A 60-year-old man with bipolar disorder on long-term lithium presents with excessive thirst and nocturia. Urine remains dilute despite rising serum osmolality. Water deprivation test: no response to desmopressin. Diagnosis: Nephrogenic diabetes insipidus secondary to lithium. Management: Stop lithium if possible; consider amiloride/thiazide + NSAIDs; low-salt, low-protein diet.
- Case 3 — Primary Polydipsia Mimicking DI 🚰: A 30-year-old woman reports constant thirst and drinking >6 L/day. Exam: normal. Labs: low-normal plasma sodium, urine osmolality increases significantly with water deprivation test. Diagnosis: Psychogenic (dipsogenic) polydipsia, not true DI. Management: Behavioural modification, psychiatric input; avoid unnecessary desmopressin (risk of hyponatraemia).
Teaching Commentary 🧠
Diabetes insipidus = impaired water reabsorption due to ADH deficiency (central) or renal resistance (nephrogenic). - Central DI: trauma, surgery, pituitary tumour, idiopathic. - Nephrogenic DI: lithium, hypercalcaemia, hypokalaemia, inherited. - Dipsogenic: excessive fluid intake mimics DI. Dx: Water deprivation test → central DI responds to desmopressin, nephrogenic does not, primary polydipsia concentrates with deprivation alone. Mx: Desmopressin for central; remove offending drugs + thiazides/amiloride for nephrogenic; behavioural therapy for dipsogenic.