Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Temporal (Giant Cell GCA) Arteritis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: | Temporal (Giant Cell GCA) Arteritis | Tocilizumab
🩺 Giant Cell Arteritis (GCA) is a large-vessel vasculitis and ophthalmological emergency. ⚠️ Can cause irreversible blindness (20% of cases) but preventable if diagnosed and treated promptly. Commonly seen in rheumatology, ophthalmology, and stroke/TIA clinics.
| 🚨 Ophthalmological Emergency – Immediate Actions |
|---|
|
💡 Tocilizumab: Humanised monoclonal antibody targeting the IL-6 receptor. Used in GCA for relapse prevention and steroid-sparing, given as weekly SC injections.
ℹ️ About GCA
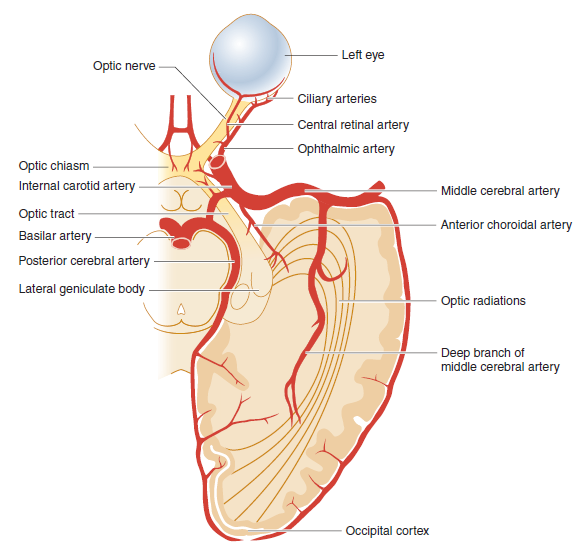
- 🎯 Vasculitis of large/medium arteries, especially branches of the external carotid (temporal, ophthalmic, ciliary, retinal).
- 👁️ Blindness risk due to anterior ischaemic optic neuropathy from posterior ciliary artery occlusion.
- 🧑🦳 ~50% overlap with Polymyalgia Rheumatica (PMR).
📊 Epidemiology
- Mean age of onset ~70 yrs; rare <50.
- ♀:♂ ratio ≈ 3:1.
- Most common in Caucasians, Northern Europeans.
🔎 Phenotypes
- 🧠 Cranial GCA (cGCA): Headache, scalp tenderness, jaw claudication, visual loss.
- 🫀 Extracranial GCA (ecGCA): Limb claudication, systemic features, aortic involvement.
- ⚖️ Mixed: Combination of both.
🩸 Vessels Involved
- Posterior ciliary arteries → AION → blindness.
- Central retinal artery → sudden visual loss.
- Extraocular muscle ischaemia → diplopia.
- Aorta may be affected → aneurysm/dissection later.
🧬 Aetiology & Pathogenesis
- Cause unclear – immune response to unidentified antigen.
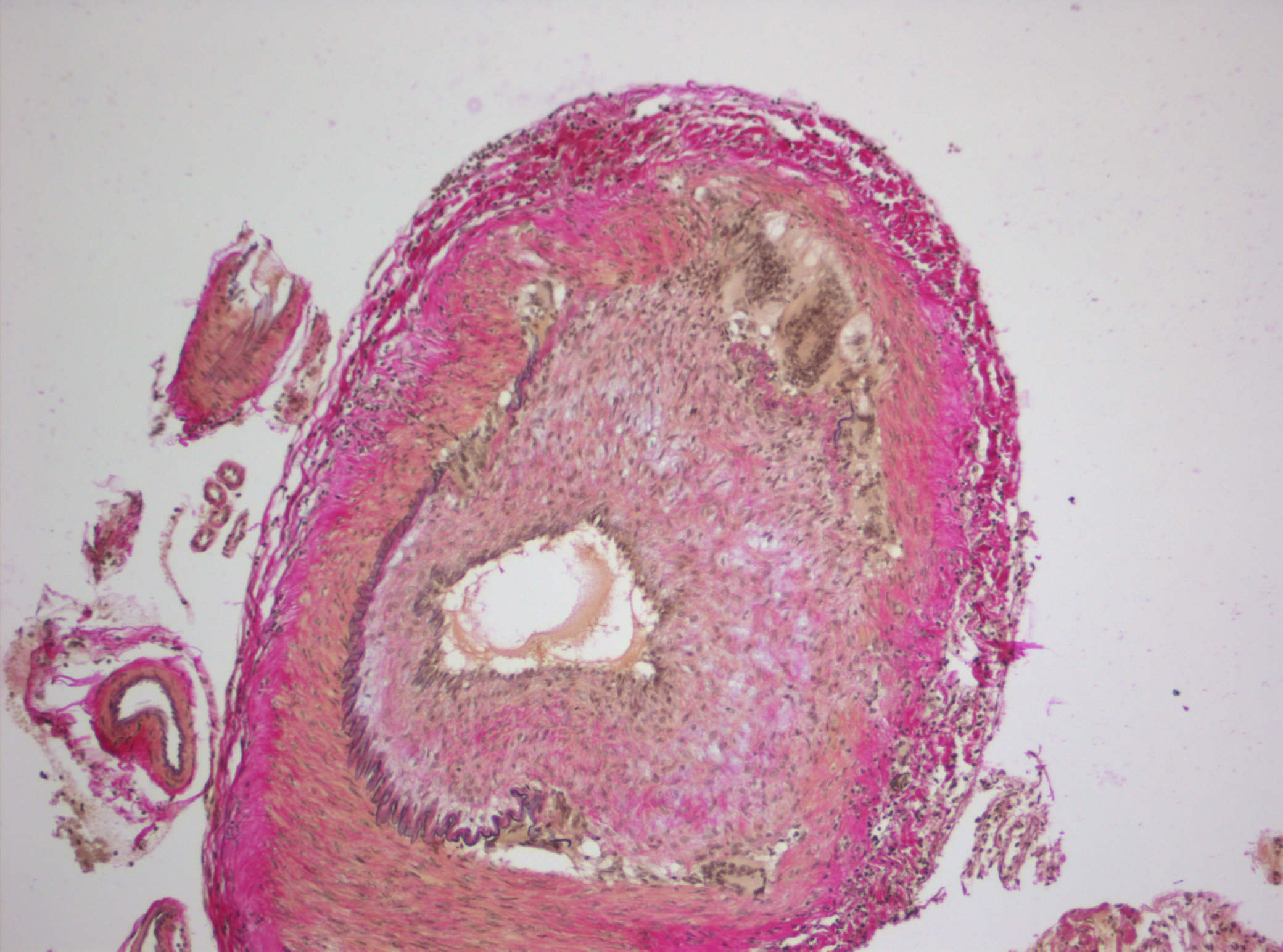
- Chronic granulomatous inflammation with multinucleated giant cells.
- Driven by Th1-mediated response, ↑ IL-6 levels central.
- Genetic: HLA-DRB1 association increases susceptibility.
📋 ACR Diagnostic Criteria (≥3/5 = GCA)
| 1 | Age ≥50 years |
| 2 | New-onset localized headache |
| 3 | Temporal artery tenderness or decreased pulse |
| 4 | Biopsy: mononuclear or granulomatous arteritis ± giant cells |
| 5 | ESR >50 mm/h (CRP often more sensitive) |
| Sensitivity ~93%, Specificity ~91%. | |
🩺 Clinical Presentation
- 🌡️ Systemic: Fever, weight loss, malaise, fatigue.
- 👁️ Visual: Transient/monocular visual loss, AION, diplopia.
- 🧠 Headache: Abrupt, often unilateral, temporal or occipital.
- 🖐️ Temporal artery: Tender, thickened, pulseless.
- 🦷 Jaw claudication (masseter ischaemia) = highly specific.
- 🚫 Stroke rare (internal carotid usually spared).
- 📉 Complications: Blindness, aortitis, aortic aneurysm/dissection (late).
🔬 Investigations
- 🩸 FBC: Normocytic anaemia, thrombocytosis.
- 🔥 ESR >50, ↑ CRP (more sensitive). ALP ↑ in 30%.
- 🖥️ Duplex US: “Halo sign” = hypoechoic wall thickening. Resolves after steroids.
- 🔬 Gold standard: Temporal artery biopsy (long segment; skip lesions common). Ideally <2 weeks after steroids.
- 👁️ Fluorescein angiography: Choroidal hypoperfusion.
💊 Management
- 👁️ Visual symptoms: Start high-dose steroids (Prednisolone 60 mg/day or 1 mg/kg). Urgent ophthalmology input. Add PPI & bone protection.
- Non-visual symptoms: Start steroids, rheumatology follow-up.
- ⏳ Taper steroids slowly over 18–24 months. Monitor relapses.
- 🧬 Tocilizumab (IL-6 inhibitor): Steroid-sparing option; SC 162 mg weekly.
- 🦴 Long-term: Bone protection, fracture prevention, cardiovascular risk management.
📚 References
- Hassan N et al. Giant Cell Arteritis. BMJ 2011;342:d3019.
Case 1 – Classic cranial GCA with visual risk
A 71-year-old woman presents with a new, severe unilateral temporal headache, scalp tenderness when brushing hair, and jaw claudication; she reports transient amaurosis fugax in the right eye. Exam shows a tender, thickened temporal artery; vision is 6/9 with a relative afferent pupillary defect. Bloods: CRP 78 mg/L, ESR 92 mm/h; platelets high-normal. Treat immediately (don’t delay for tests) with high-dose glucocorticoids—if visual symptoms, give IV methylprednisolone 500–1000 mg daily × 3 then switch to oral prednisolone 40–60 mg daily with PPI and bone protection; add low-dose aspirin if no contra-indication. Arrange urgent temporal artery ultrasound (halo sign) and/or biopsy within 7 days, plus ophthalmology review; baseline glucose/BP/DEXA and plan a slow taper with rheumatology follow-up. Watch for complications: arteritic AION, stroke, aortic aneurysm.
Case 2 – Polymyalgia phenotype with dull headache systemic features
A 68-year-old man with 4 weeks of proximal shoulder/hip girdle pain and morning stiffness develops low-grade fever, weight loss, and new dull headache without jaw pain. Exam: reduced active abduction, no overt temporal artery tenderness. Bloods: CRP 56, ESR 70; mild normocytic anaemia. Given red flags for GCA in a PMR-like presentation, start prednisolone 40 mg daily the same day; symptoms improve within 48 hours, supporting the diagnosis. Arrange temporal artery ultrasound (± biopsy) and consider large-vessel imaging (CTA/MRA) to assess aorta. Add calcium/vitamin D, bisphosphonate if at risk; screen for steroid toxicity and consider steroid-sparing therapy (e.g., methotrexate or tocilizumab in refractory/relapsing disease) under rheumatology. Educate on urgent return if visual change, jaw claudication, or limb ischaemia develops.
Case 3 – Pure Polymyalgia Rheumatica (no GCA features)
A 73-year-old woman reports 3 weeks of bilateral shoulder and hip girdle pain with morning stiffness >60 minutes, difficulty rising from a chair, and sleep disturbance, but no headache, jaw claudication, visual symptoms, or limb ischaemia. Exam: painful but full passive ROM; no synovitis or temporal artery tenderness. Labs: CRP 48 mg/L, ESR 62 mm/h, mild normocytic anaemia; CK, TSH, Ca, RF/anti-CCP and urine dip are unremarkable. Diagnosis: PMR (after excluding mimics—rotator cuff disease, OA, hypothyroidism, myeloma, infection, malignancy). Start prednisolone 12.5–15 mg daily with a structured taper over months, review in 1–2 weeks for >70% symptom and CRP/ESR response; add bone protection (vitamin D ± bisphosphonate as per FRAX), GI and diabetes risk mitigation, and vaccinations. Safety-net: urgent assessment if any GCA red flags develop; consider methotrexate if relapsing/steroid-intolerant; involve rheumatology if atypical course.