Related Subjects:Pneumonia
|Pontiac fever (Legionella Pneumophila)
|Legionella Pneumophila pneumonia
|Asthma
|Acute Severe Asthma
|Exacerbation of COPD
|Pulmonary Embolism
|Cardiogenic Pulmonary Oedema
|Pneumothorax
|Tension Pneumothorax
|Respiratory (Chest) infections Pneumonia
|Fat embolism
|Hyperventilation Syndrome
|ARDS
|Respiratory Failure
|Diabetic Ketoacidosis
|Breathlessness
You must know about CURB65 scoring for Community-acquired pneumonia. Atypical pneumonias have unusual presentations e.g. with headache and a viral meningitis picture, diarrhoea, vomiting, abdominal pain, myalgia and the chest symptoms may take time to appear both clinically and radiologically
About
- Infection of the air spaces and substance of the lung which are normally sterile
- Lobar - restricted to the whole of one lobe ? is there a bronchostenotic lesion
- Bronchopneumonia - affecting lobules and bronchi
Aetiology
- Classification depends on location as different organisms
- Community acquired - symptoms + signs of consolidation
- Hospital acquired - onset >48 hours after admission.
Organisms numbers vary by study, age group, other pathologies
| Organism | Details | Investigations | Treatment |
|---|
| Streptococcus pneumoniae | Commonest. Middle aged. Cough with green/rusty sputum, fever, pleurisy. Associated HSV cold sores. Main cause of lobar pneumonia. Cavities with serotype 3 | Sputum, blood and urine - pneumococcal antigen | Penicillin (if allergic, Erythromycin) e.g. Treat with Benzyl Penicillin 1-2 g 6 hrly
|
| Mycoplasma pneumoniae | Children and young adults. Autumnal and 3-4 year epidemic cycle Atypical pneumonia - cough and sputum absent in 1/3 cases. Preceding flu-like symptoms usually, e.g. headache, myalgia, GI upset before the onset of respiratory symptoms Myocarditis, pericarditis, erythema multiforme, haemolytic anaemia, myalgia, arthralgia,
meningoencephalitis, cold agglutinins | Serology for IgM and IgG antibodies (acute and convalescent titres), cold
agglutinins (in 50%). | Erythromycin, Azithromycin, Clarithromycin or
Doxycycline
|
| Haemophilus influenzae |
Especially seen in the elderly, heavy smokers and COPD patients |
No specific features; may be broncho- or lobar pneumonia |
Cefuroxime or Co-Amoxiclav
|
| Moraxella catarrhalis |
Common cause of bronchopneumonia especially in the elderly and COPD
patients | No specific features; may be
broncho- or lobar pneumonia | Cefuroxime or Co-Amoxiclav
|
| Staphylococcus aureus |
More common following influenza pneumonia, IV drug, central line Severe pneumonia, post-influenza may be rapidly fatal. Abscess formation, pneumothorax, empyema relatively common. Septicaemia: infective emboli causing abscesses in other organs. |
Nodular consolidation and cavitation on CXR. | Flucloxacillin
|
| Chlamydia psittaci 'Psittacosis' | Acquired from avian excreta seen in those exposed to birds. Malaise, high fever, dry cough, hepatosplenomegaly and rose spots on the abdomen. Hepatitis, encephalitis, renal failure. Hepatosplenomegaly. | Serology for Chlamydia antibodies - complement-fixing antibodies (immunofluorescent
tests to distinguish types). | Erythromycin, Azithromycin, Clarithromycin or Doxycycline
|
| Chlamydophila pneumoniae | Causes 5-10% of
community acquired Often mild flu-like illness or acute bronchitis recovering
spontaneously. Pneumonia also usually mild
| CXR: Segmental Infiltrates, Acute and convalescent sera | Erythromycin,
Azithromycin, Clarithromycin or Doxycycline
|
| Coxiella burnetii (Q fever) | Only 1% of cases overall Influenza-like illness which causes a pneumonia if it persists, often with multiple CXR lesions
Endocarditis. If untreated chronic infection is fatal |
Serology - complement fixing antibody. CXR: Multiple segmental shadows |
Erythromycin, Azithromycin, Clarithromycin or Doxycycline Hypoalbuminaemia and
abnormal LFTs (raised transaminases) are common. Acute renal failure.
|
| Legionella pneumophilia | Infection from water system. Sporadic cases source unknown. Middle-aged and older, Recent travel, Autumn time. Outbreaks in immunocompromised
individuals. x 2 in Males. Usually 2-10 day prodromal of dry cough, confusion, headache, myalgia or diarrhoea, low WCC, Low Na, abnormal LFTs. CR shadows.
| Urine for specific antigen. Immunofluorescent tests on sputum or
bronchial lavage. |
Erythromycin, Azithromycin,
Clarithromycin or Ciprofloxacin +/? Rifampicin Despite
these mortality 20%
|
| Klebsiella | Elderly with a history of
heart or lung disease,
diabetes, alcohol
excess or malignancy
Sudden onset, severe
systemic upset, purulent,
mucoid sputum
(classically red currant
jelly). Lobar pneumonia |
CXR : cavitating lesions
- lung abscesses
Extensive lobar
consolidation with
cavitation. Widespread consolidation (upper lobes) |
Cefuroxime and
Gentamicin
|
| Pseudomonas
aeruginosa |
Nosocomial, cystic
fibrosis and
neutropenic patients. |
Sputum and blood culture |
but it does colonise the
upper airway as a
commensal
Ciprofloxacin or
ceftazidime
Anaerobes -
Bacteroides
Aspiration, e.g. due to
stroke. Diabetics
Metronidazole
|
| Pneumocystis
jiroveci (PCP)
(Previously
Pneumocystis
carinii) |
The most common
opportunistic
infection in AIDS
(CD4 count
<200/mm3) and
immunosuppressed
patients
High fever, dry cough,
shortness of breath,
tachycardia. Marked
hypoxia, particularly
following exertion. Fine
crackles or nothing to
find on auscultation.
Mortality now 10%
| Typical CXR - perihilar
'butterfly' ground glass
shadowing. but may be
normal in early disease.
CT shows ground-glass
shadowing, bronchial
lavage or induced
sputum for diagnosis by
silver staining or by
immunofluorescence |
Long-term prophylaxis is required, e.g. with co-trimoxazole Hi-dose i.v. cotrimoxazole or i.v. pentamidine
|
| Viral Pneumonia | Influenza, Parainfluenza, Measles, RSV in infants, Varicella can cause severe pneumonia with multiple miliary nodular shadows which may calcify | Relevant serology | Consider Neuraminidase inhibitors if Influenza |
Types
- Community acquired Pneumonia - at-risk groups : Aspiration (Stroke, MND), Alcohol, Diabetes, Steroids/Immunosuppression, Smokers, COPD, Nursing home residents
- Hospital acquired - same as CAP. Elderly, immunosuppressed, respiratory disease, post-operative, ITU. Usually Gram-negative enterobacteria - pseudomonas, klebsiella and Anaerobes
Risk Groups
- Cigarette smoking and underlying lung disease.
- Stroke or other neuromuscular disorder (aspiration pneumonia often by anaerobes).
- Immunosuppression and AIDS in particular P.
jirovecii.
- Intravenous drug abusers, Alcoholics and vagrants.
- Hospital patients (more often Gram-negative organisms).
Pathology stages
- 1. Congestion and vascular engorgement and alveolar bacteria
- 2. Red hepatization - alveolar spaces full of polymorphous and fibrin and red cells
- 3. Grey hepatization - RBC breakdown, fibrin and suppurative inflammation
- 4. Resolution - exudate removed by macrophages
Clinical
- Fever, sweats, rigors, Dry cough initially, malaise
- Confusion, Delirium (elderly and Legionella)
- Breathlessness, Cyanosis
- Tachycardia, Hypotension
- Pleuritic type chest pain
- Cough, Rusty sputum (Pneumococcus) yellow/green sputum
- Haemoptysis
- Flare up of herpes simplex (Pneumococcus)
- Atypical - diarrhoea, myalgia, headache
- Reduced air entry and expansions and dullness to percussion
- Increased vocal resonance
- Stony dull if effusion/empyema
Complications
- Abscess formation, Pleural effusion
- Parapneumonic effusion and Empyema
- Bacteraemia, Sepsis
- Cerebral abscess, Meningitis
- ARDS, Respiratory Failure, Cardiac Failure, Death
Investigations
- Sputum - gram stain and culture and sensitivity is not recommended for patients in the community. Is useful for those who do not respond to empirical therapy. In hospital, sputum should be sent. The sample should be obtained from a deep cough and should be grossly purulent The sample should be transported promptly to the laboratory for processing. A purulent portion of the sputum should be selected for Gram stain and culture Cytological screening should be done as a contingency for culture The sample should be cultured using standard techniques Interpretation should be based on the correlation of Gram stain, semi-quantitative culture results and clinical picture
- FBC - elevated WCC. Low WCC with legionella.
- Pulse oximetry: An oxygen saturation (SaO₂) of <92% defines hypoxaemia (grade A-), and patients with SaO₂ <92% should have an arterial blood gas measurement
- Blood film - red cell agglutination suggests cold agglutinins and Mycoplasma
- ESR and CRP elevated
- U&E - raised urea, low Na with legionella
- LFT'S - abnormal with legionella
- Blood cultures and sensitivities
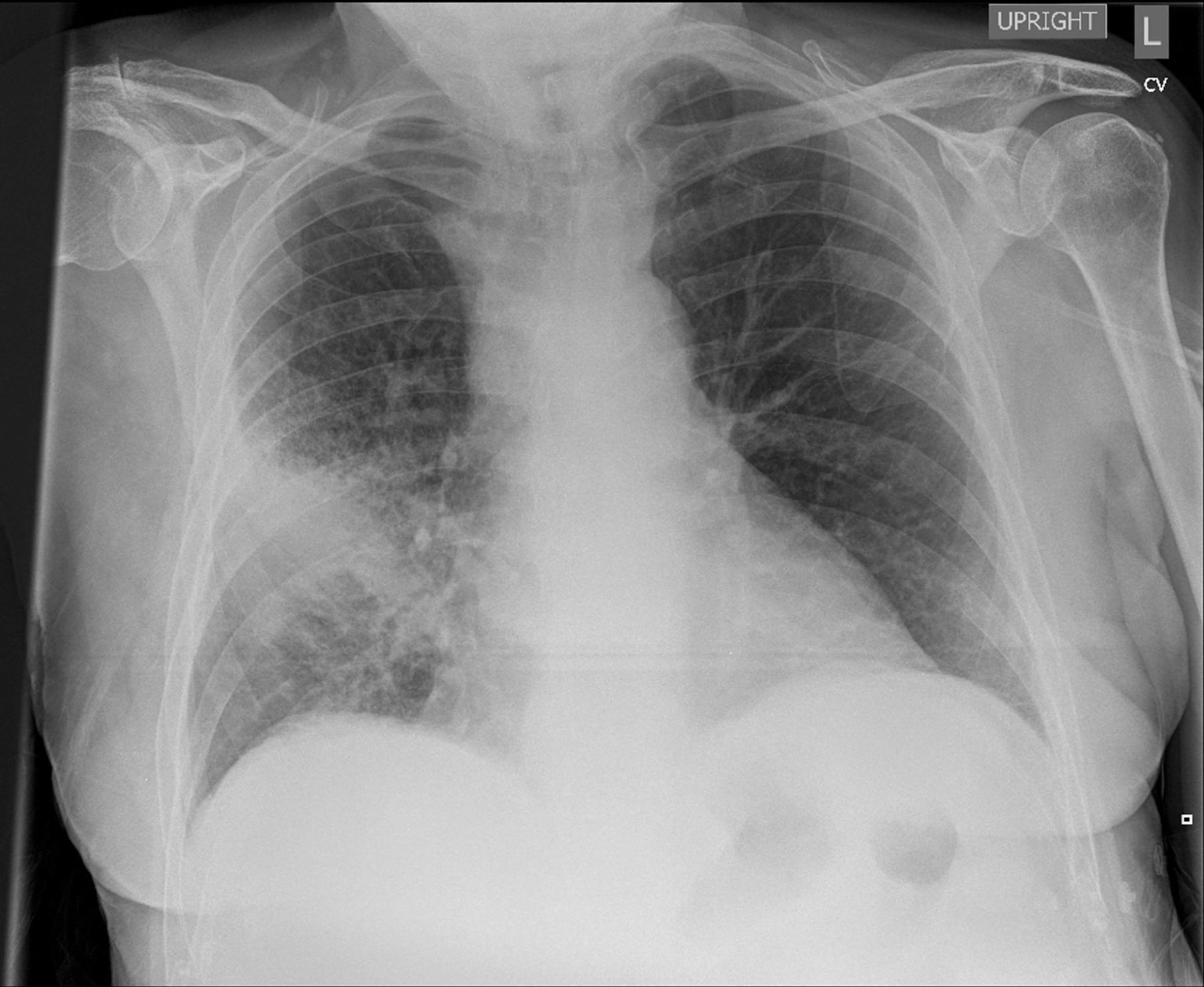
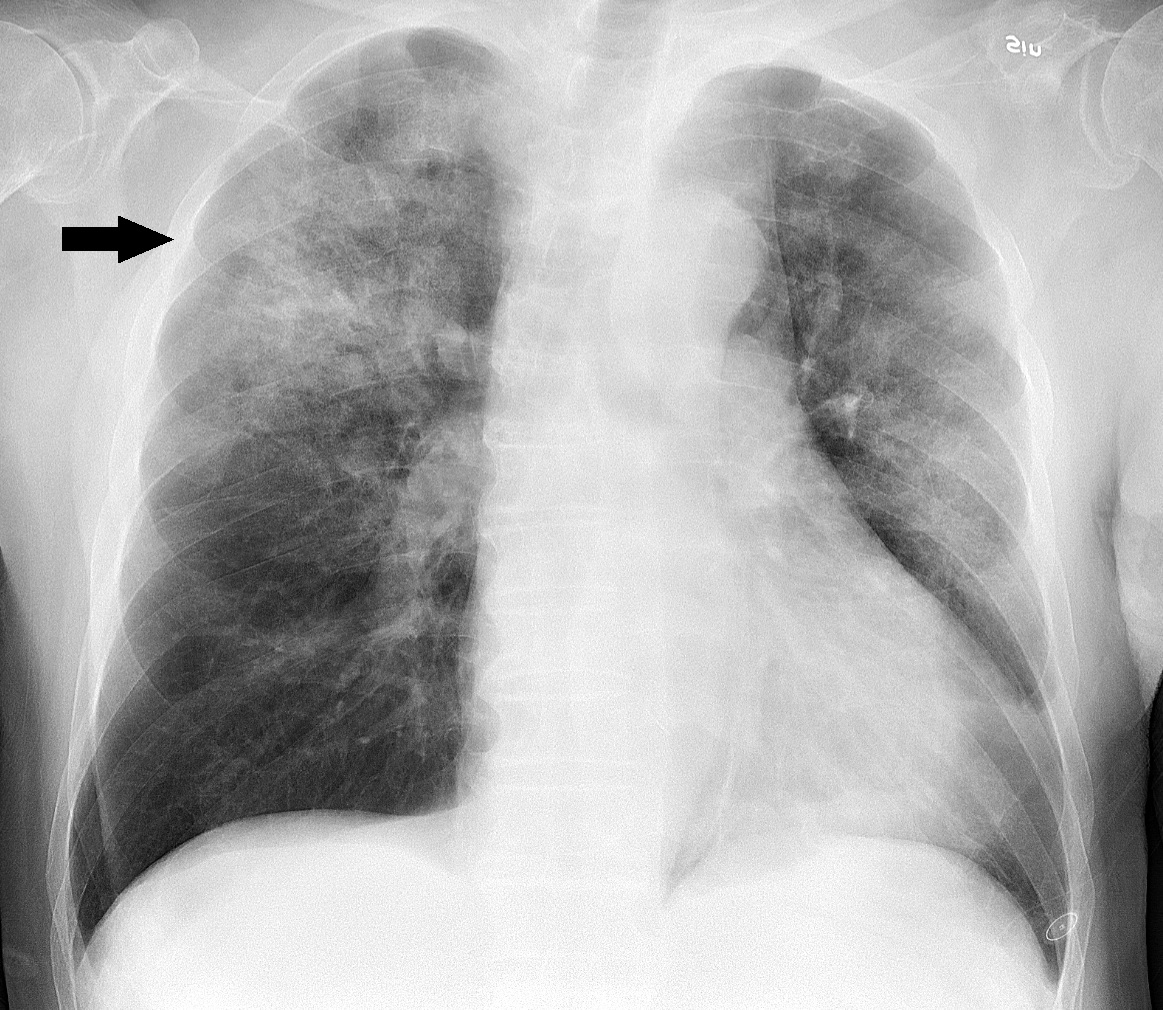
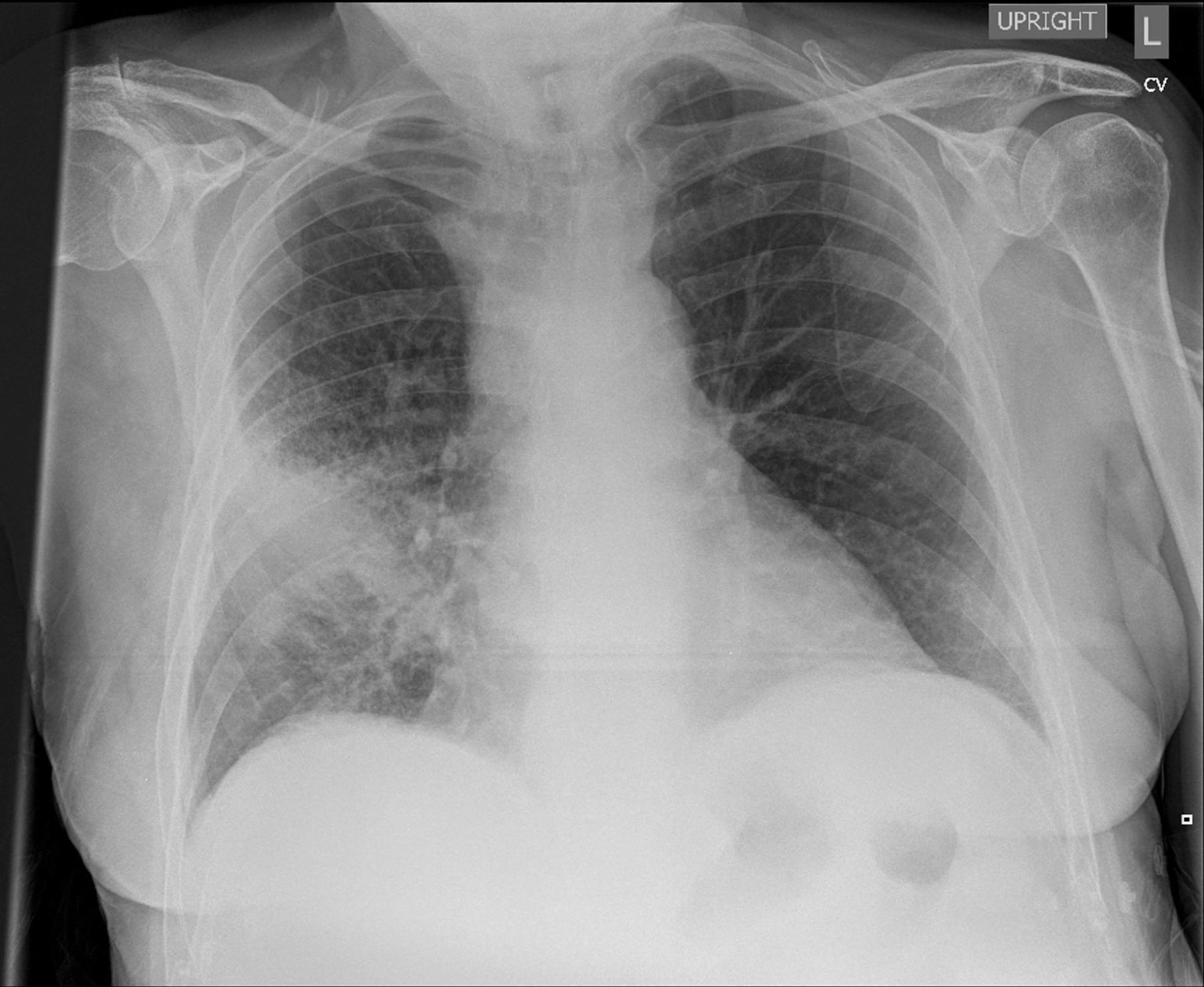
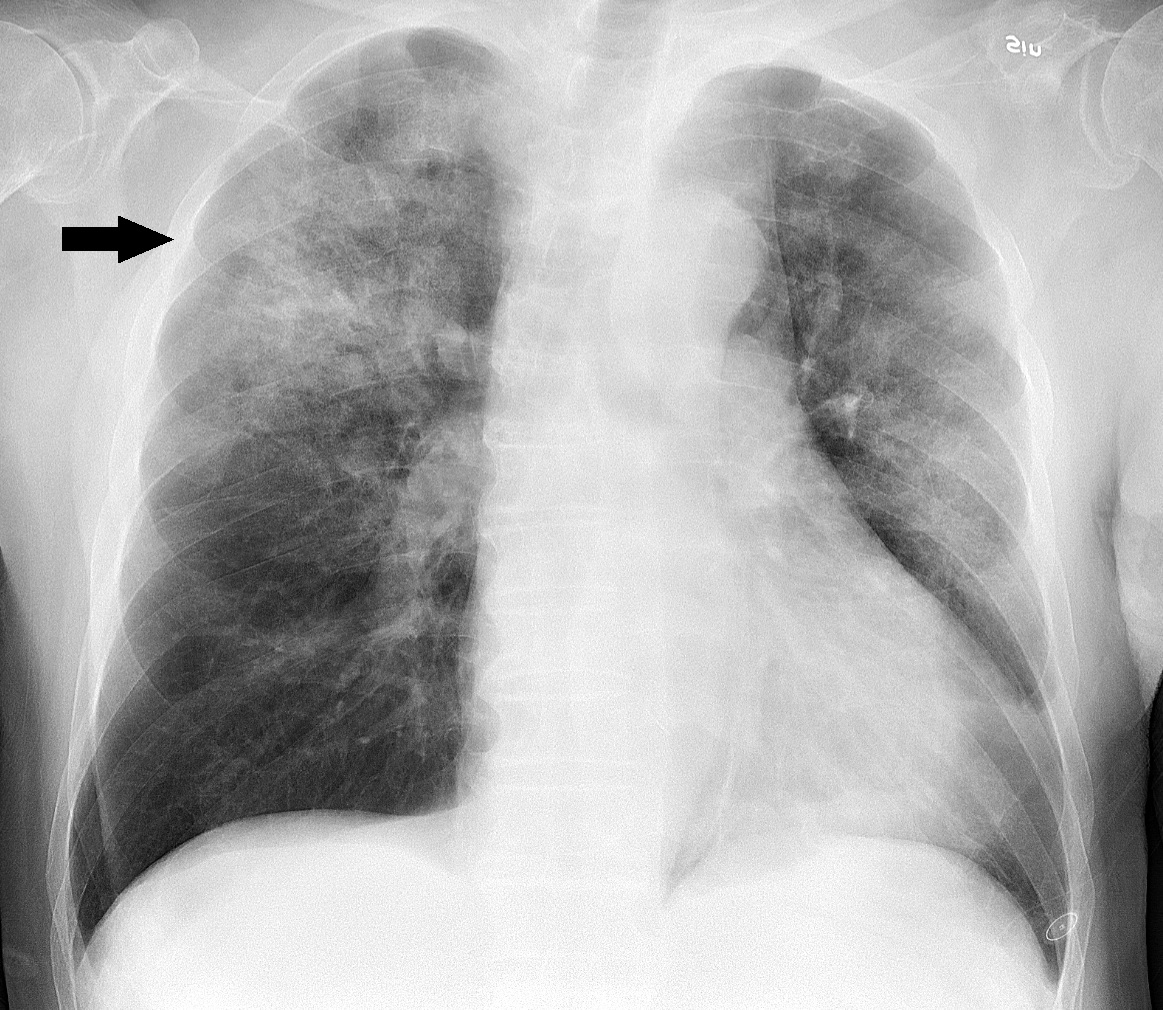
- CXR - patchy consolidation with bronchopneumonia. More defined consolidation with lobar pneumonia. Cavitation may be seen, parapneumonic effusion. Changes often lag behind clinical changes. Not recommended in those managed in the community (BTS). Watch out that CXR may be normal in the first 24 hours in cases of severe neutropenia (no inflammatory response) and in Pneumocystis pneumonia
- Arterial blood gas - hypoxia and possibly hypercarbia with V/Q mismatch
- Serology - Mycoplasma, Chlamydia, Coxiella, Influenza, Adenoviral, RSV
- Legionella: Urine test for legionella antigens in any high-severity CAP
- Pneumococcus: Urinary testing for Pneumococcus in those with moderate or high-severity CAP
- Bronchoscopy in some cases to look for any broncho stenotic lesions or remove foreign bodies or mucus plugging
- CT chest - to look for other related pathology
Differentials
- Pulmonary embolism: breathlessness (about 75% of cases) , pleuritic pain (about 66% of cases) and cough (about 33% of cases
- Spontaneous pneumothorax typically presents with pleuritic chest pain and breathlessness
- Pulmonary oedema
- ARDS, Pulmonary haemorrhage
- Cryptogenic organising pneumonia
- Lung cancer
- Acute extrinsic allergic alveolitis
CURB Scoring
| CURB Scoring - consider all of these |
|---|
| Confusion - MTS of 8 or less, or new disorientation in person, place or time | +1 |
| Urea >7 mmol/l | +1 |
| Respiratory rate >30/min | +1 |
| Blood pressure (SBP < 90 mmHg or DBP < 60 mmHg) | +1 |
| Age >65 years Score 1 point for each feature present | +1 |
| Points from CURB-65 |
|---|
| 0/1: Likely suitable for home treatment |
| 2:Consider hospital supervised treatment. Options may include a) short stay in-patient or b) hospital supervised out-patient |
| 3+ :Manage in hospital as severe pneumonia Assess for ICU admission especially if CURB-65 score = 4 or 5 |
Additional evidence of severity
- Hypoxaemia < 8Kpa
- WCC >20 or < 4
- CXR - multi lobe involvement on CXR
- Albumin < 35 g/L
- Microbiology - positive blood culture
- Others - stroke, COPD, cardiac disease, diabetes
Management
- Start with 28% in COPD use 35-40% if no COPD and repeat ABG. Oxygen - aim for PO₂ >8 Kpa
- IV fluids - hydration important but avoid overload in elderly or with CCF
- May need CPAP, BIPAP, or ITU if worsening respiratory failure
- Aspirate pleural effusions and If the fluid looks turbid, a chest tube should be inserted promptly for empyema



All patients need follow up CXR or CT follow up radiology at 6 weeks to ensure complete resolution and no underlying pathology
Antibiotic management
Offer an antibiotic(s)
within 4 hours of establishing a diagnosis. When microbiological results available: review the choice of antibiotic(s), and change the antibiotic(s) according to results, using a narrower spectrum antibiotic, if appropriate. If fails to improve Seek specialist advice from a microbiologist
- First-choice oral antibiotic if low severity (based on clinical judgement and guided by CRB65 score 0, or CURB65 score 0 or 1
- Amoxicillin 500 mg 3 times a day (higher doses can be used see BNF) for 5 days
- Consider adding a macrolide to Amoxicillin if atypical pathogens are suspected.
- Alternative oral antibiotics if low severity, for penicillin allergy or if Amoxicillin unsuitable (for example, atypical pathogens suspected)
- Doxycycline 200 mg on first day, then 100 mg once a day for 4 days (5-day course) then review
- Clarithromycin 500 mg twice a day for 5 days
- Erythromycin (in pregnancy) 500 mg 4 times a day for 5 days
- First-choice oral antibiotics if moderate severity (based on clinical judgement and guided by CRB65 score 1 or 2, or CURB65 score 2); guided by microbiological results when available
- Amoxicillin with (if atypical pathogens suspected):
500 mg 3 times a day (higher doses can be used see BNF) for 5 days
- Clarithromycin 500 mg twice a day for 5 days OR
- Erythromycin (in pregnancy) 500 mg 4 times a day for 5 days
- Alternative oral antibiotics if moderate severity, for penicillin allergy; guided by microbiological results when available
- Doxycycline 200 mg on first day, then 100 mg once a day for 4 days (5-day course in total)
- Clarithromycin 500 mg twice a day for 5 days
- First-choice antibiotics if high severity (based on clinical judgement and guided by CRB65 score 3 or 4, or CURB65 score 3 to 5); guided by microbiological results when available
- Co-Amoxiclav 500/125 mg 3 times a day orally or 1.2 g 3 times a day IV for 5 days WITH
- Clarithromycin 500 mg twice a day orally or IV for 5 days
OR
- Erythromycin (in pregnancy) 500 mg 4 times a day orally for 5 days
- Alternative antibiotic if high severity, for penicillin allergy; guided by microbiological results when available
- Levofloxacin (consider safety issues) 500 mg twice a day orally or IV for 5 days
- Consult local microbiologist if fluoroquinolone not appropriate.
References