Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Accelerated Idioventricular Rhythm
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🫀 Accelerated Idioventricular Rhythm (AIVR) is a transient ventricular rhythm often seen post-MI, particularly during reperfusion. It is usually benign, self-limiting, and haemodynamically well tolerated, so treatment is rarely required. The key challenge is distinguishing it from slow VT or CHB.
📖 About
- Commonly observed after reperfusion in acute MI (PCI or thrombolysis).
- Often resembles a "slow VT" but is not typically malignant.
- Most cases resolve spontaneously as sinus rate accelerates past the ventricular focus.
- Generally requires only observation and reassurance unless instability develops.
📊 ECG Characteristics
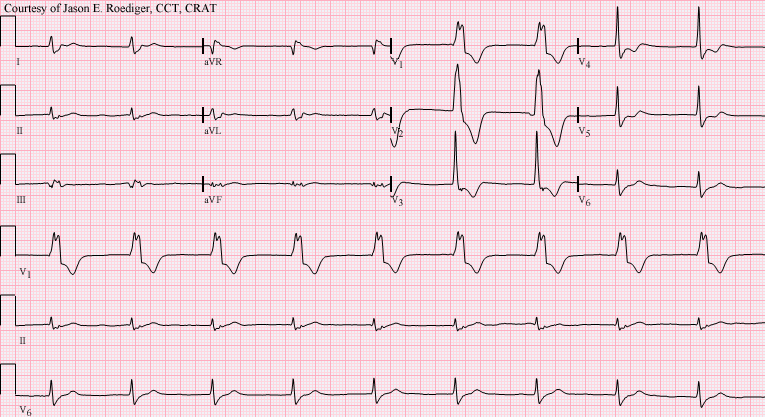
- Broad-complex rhythm, usually regular.
- Rate: 40–120 bpm (classic: 60–100). 🕒
- AV dissociation often present (cannon A waves may be seen clinically).
- At rates >110–120 bpm, consider slow VT instead.
🧾 Differential Diagnosis
- CHB with escape rhythm: if rate <50 bpm.
- Slow VT: if rate >110–120 bpm, particularly in scarred ventricles.
- Junctional rhythm with aberrancy: consider if QRS morphology varies.
⚠️ Causes / Associations
- 💔 Acute STEMI, especially reperfusion arrhythmia.
- Ischaemic heart disease, cardiomyopathy.
- Myocarditis, digoxin toxicity (check K⁺ and drug levels).
- Cocaine use.
- Normal finding in well-trained athletes (high vagal tone).
- During ROSC after cardiac arrest.
🩺 Clinical Features
- Often asymptomatic, may have variable heart sounds due to AV dissociation.
- Seen in acute MI context → always check for associated complications.
- Usually haemodynamically stable (key teaching pearl: instability is unusual).
💊 Management
- Observation only in most cases – treat the underlying condition (e.g., MI).
- Spontaneously resolves once sinus node regains dominance.
- Do NOT suppress with antiarrhythmics (lidocaine, amiodarone) unless unstable – risk of asystole ⚠️.
- Seek senior input if in doubt, particularly in the peri-MI setting.
📚 References
Cases — Accelerated Idioventricular Rhythm (AIVR)
- Case 1 — Post-Reperfusion MI: A 58-year-old man is admitted with an acute anterior STEMI. He undergoes primary PCI with stenting of the LAD. An hour later, telemetry shows a wide-complex rhythm at 70 bpm with gradual onset and offset. He is asymptomatic, BP stable, and the rhythm spontaneously reverts to sinus. Diagnosis: AIVR following reperfusion therapy for MI. Management: No treatment needed — benign rhythm. Monitor and continue post-MI care (dual antiplatelets, beta-blocker, ACEi, statin).
- Case 2 — Digoxin Toxicity: A 72-year-old woman with atrial fibrillation on digoxin presents with nausea and visual halos. ECG: regular wide-complex rhythm at 60 bpm, independent of atrial activity. Serum digoxin level high. Diagnosis: AIVR associated with digoxin toxicity. Management: Stop digoxin, correct electrolytes (especially potassium and magnesium), consider digoxin-specific antibody fragments if severe. Continuous cardiac monitoring until rhythm resolves.
Teaching Commentary ⚡
AIVR is a ventricular rhythm faster than the intrinsic ventricular escape rate (≈40 bpm) but slower than VT (usually 50–110 bpm). It typically occurs after reperfusion of acute MI (a “reperfusion arrhythmia”), but also in drug toxicity (digoxin), cardiomyopathy, and metabolic disturbances. ECG shows a regular, wide-complex rhythm with gradual onset/offset. Unlike VT, AIVR is benign and self-limiting, rarely requiring treatment. Management is to treat the underlying cause (e.g. reperfusion, stop digoxin, correct electrolytes) rather than antiarrhythmics.