Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Ascites
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Chronic liver disease |Cirrhosis |Alkaline phosphatase (ALP) |Liver Function Tests |Ascites Assessment and Management |Budd-Chiari syndrome |Autoimmune Hepatitis |Primary Biliary Cirrhosis |Primary Sclerosing Cholangitis |Wilson disease |Hereditary Haemochromatosis |Alpha-1 Antitrypsin (AAT) deficiency |Non alcoholic steatohepatitis (NASH) |Spontaneous Bacterial Peritonitis |Alcoholism and Alcoholic Liver Disease
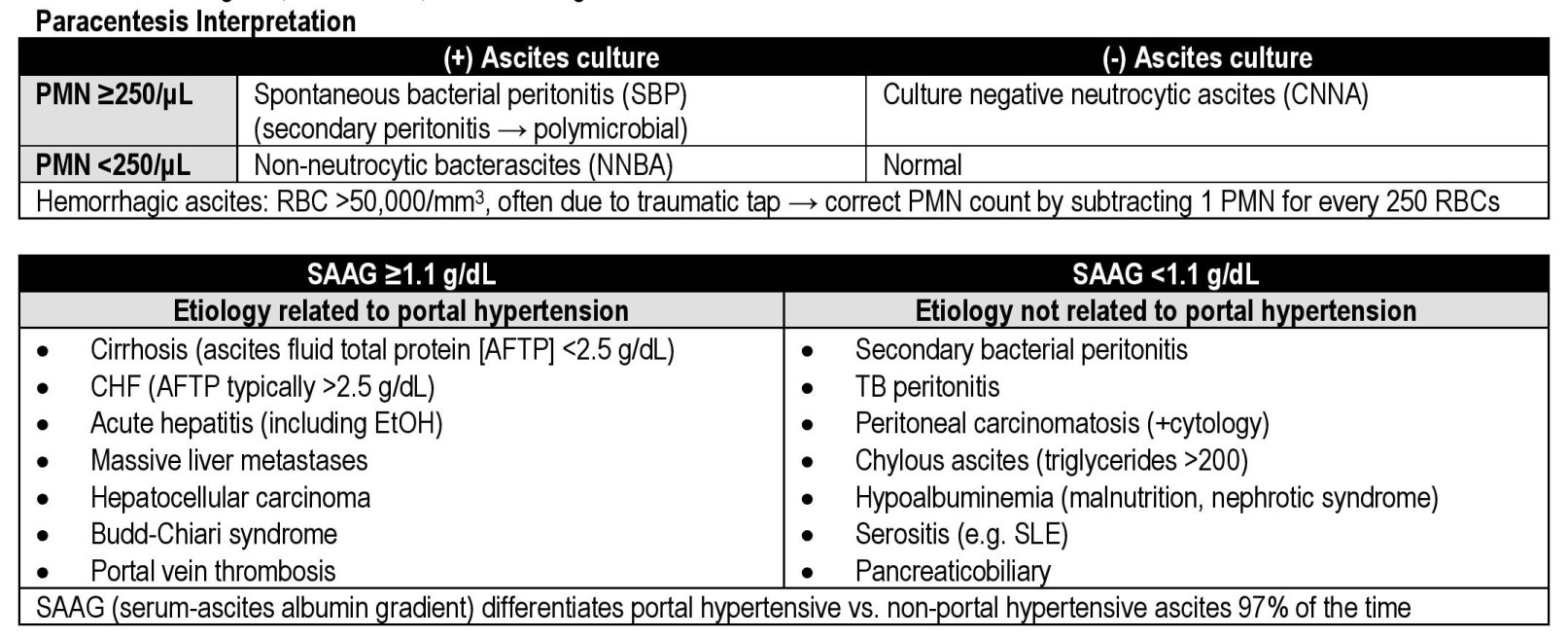
💧 The Serum-Ascites Albumin Gradient (SAAG) helps determine the cause of ascites: 👉 SAAG ≥ 11 g/L → due to portal hypertension (e.g. cirrhosis, heart failure). 👉 SAAG < 11 g/L → due to non-portal causes (e.g. malignancy, TB, pancreatitis).
📌 About Ascites
- 🧾 Definition: Pathological accumulation of fluid in the peritoneal cavity.
- 📊 Common Causes: Cirrhosis (~80%), malignancy, heart failure, nephrotic syndrome, TB.
- 😮💨 Presentation: Progressive abdominal distension, discomfort, bloating, dyspnoea from diaphragmatic splinting.
🔎 Aetiology
- 🫀 Portal Hypertension: Cirrhosis, Budd–Chiari, right heart failure.
- 🧪 Hypoalbuminaemia: Nephrotic syndrome, cirrhosis → ↓ oncotic pressure.
- 💊 RAAS Activation: Sodium/water retention exacerbates fluid overload.
- 🦠 Malignancy & Infection: Peritoneal carcinomatosis, TB peritonitis.
👩⚕️ Clinical Features
- 🫃 Distended abdomen with bulging flanks.
- 🔄 Shifting dullness (needs >1.5 L fluid).
- 🌊 Fluid thrill (requires >2 L).
- Associated: fatigue, bloating, SOB, early satiety.
🧪 Investigations
| SAAG | Likely Cause |
|---|---|
| ≥ 11 g/L (high gradient) | Portal HTN (cirrhosis, cardiac ascites, Budd–Chiari) |
| < 11 g/L (low gradient) | Peritoneal causes (malignancy, TB, pancreatitis, nephrotic syndrome) |
- 💉 Ascitic fluid analysis:
- Cell count → neutrophils >250/mm³ = SBP.
- Protein → low in cirrhosis, high in infection/malignancy.
- Cytology for malignant cells.
- Glucose ↓ in TB/malignancy, Amylase ↑ in pancreatitis.
- 🖥️ Ultrasound: Detects 100–200 ml fluid (clinical exam needs >1.5 L).
- 🩻 CXR/CT: Look for hepatomegaly, peritoneal masses, bowel disease.
💊 Management
- 🍽️ Conservative: Na⁺ restriction (≤2 g/day), bed rest, daily weights.
- 💊 Diuretics: Spironolactone ± furosemide (monitor U&E).
- 💉 Therapeutic paracentesis:
- <5 L drained → no albumin required.
- ≥5 L drained → give 8 g IV 20% albumin per L removed.
- 🔄 Refractory ascites: Consider TIPS.
- 🩺 Definitive: Liver transplant if eligible.
- 🦠 SBP prophylaxis: Norfloxacin/ciprofloxacin if prior SBP.
⚠️ Complications
- 🦠 Spontaneous bacterial peritonitis (SBP): Neutrophils >250/mm³ → IV cefotaxime.
- 🗂️ Hepatorenal syndrome: Functional renal failure in cirrhotics.
- 🌬️ Hepatic hydrothorax: Pleural effusion via diaphragmatic defect.
🧑⚕️ Case Examples
Case 1: 👨 A 58-year-old man with alcoholic cirrhosis presents with progressive abdominal swelling and ankle oedema. 🔎 Exam: shifting dullness. SAAG = 18 g/L. Ascitic protein is low. ✅ Managed with salt restriction, spironolactone, and therapeutic paracentesis. Referred for transplant assessment.
Case 2: 👩 A 42-year-old woman presents with abdominal distension, fever, and weight loss. 🔎 Ascitic tap: SAAG = 7 g/L, protein high, glucose low, lymphocytosis. Diagnosis: TB peritonitis. ✅ Started on anti-TB therapy and monitored closely for treatment response.
📚 References
Cases — Ascites
- Case 1 (Cirrhotic Ascites): A 58-year-old man with a history of alcohol-related liver disease presents with progressive abdominal distension, ankle oedema, and early satiety. Examination shows shifting dullness and spider naevi. Bloods reveal deranged LFTs and thrombocytopenia. Diagnostic paracentesis shows low SAAG (<1.1 g/dL) with no malignant cells. Management: Sodium restriction, spironolactone started, furosemide added later. Regular monitoring of renal function and electrolytes. Outcome: Symptom improvement with diuretics, occasional need for therapeutic paracentesis. Referred for hepatology follow-up and transplant assessment.
- Case 2 (Malignant Ascites): A 66-year-old woman with weight loss, anorexia, and abdominal bloating is found to have tense ascites. She has a past history of ovarian cancer. CT abdomen shows peritoneal nodularity. Ascitic tap reveals malignant cells. Management: Large-volume paracentesis for symptom relief, indwelling peritoneal catheter considered for recurrent accumulation. Palliative care team involvement, chemotherapy discussed but prognosis poor. Outcome: Symptomatic relief achieved; discharged with community nursing support. Died peacefully at home 4 months later.
- Case 3 (Cardiac Ascites): A 72-year-old man with long-standing right-sided heart failure presents with increasing abdominal distension and peripheral oedema. JVP raised, hepatomegaly palpable. Bloods show normal LFTs, BNP elevated. Ascitic tap: high SAAG (>1.1 g/dL), low protein. Management: Optimisation of heart failure therapy — IV furosemide, spironolactone, and fluid restriction. Treated underlying atrial fibrillation with rate control. Outcome: Gradual resolution of ascites with improved heart failure control. Discharged on optimised medical therapy and cardiology follow-up.
Teaching Commentary 🧑⚕️
Ascites is the abnormal accumulation of peritoneal fluid. The key step is identifying the cause: • Cirrhosis/portal hypertension (most common, SAAG >1.1 g/dL, high protein if cardiac, low if cirrhotic). • Malignancy (often bloody/serous, SAAG <1.1 g/dL, malignant cells on cytology). • Cardiac failure (right heart strain, raised JVP, high SAAG, low protein). Initial management includes salt restriction and diuretics; therapeutic paracentesis is used for tense or refractory ascites. Always analyse ascitic fluid (SAAG, protein, cytology, culture) to guide diagnosis. Prognosis depends on the underlying condition — poor in malignancy, variable in cirrhosis depending on transplant eligibility, and linked to cardiac disease in heart failure.