Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Splenomegaly Examination (OSCE)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Cardiology Examination
|Cardiology History Taking
|Epstein-Barr Virus infection
|Cytomegalovirus (CMV) infections
Examination of the spleen helps detect splenomegaly, assess consistency, and guide investigations. Key OSCE pearl: always start palpation in the right iliac fossa as the spleen enlarges diagonally towards it.
Mnemonic (Massive Splenomegaly): "MMM" = Myelofibrosis, Malaria, Myeloid leukaemia (CML).
Spleen exam = Inspect 👀 → Palpate ✋ (RIF→LUQ, with inspiration) → Percuss 🥁 (Traube’s space).
Normal spleen not palpable.
Massive splenomegaly → think MMM (Myelofibrosis, Malaria, Myeloid leukaemia).
Always document fully & link findings to systemic disease.
🛠️ Preparation
👀 Inspection
✋ Palpation
🥁 Percussion
📋 Common Findings
📝 Documentation
🧾 Causes of Splenomegaly
📊 Investigations
Investigation Finding
FBC Pancytopenia (hypersplenism), anaemia
Blood film Abnormal cells (e.g., blasts in leukaemia, parasites in malaria)
LFTs Signs of cirrhosis/portal hypertension
Ultrasound/CT Confirm splenomegaly, assess structure
Bone marrow biopsy Myeloproliferative / infiltrative causes
Serology Infections: EBV, malaria, kala-azar
⚕️ Management
📈 Summary
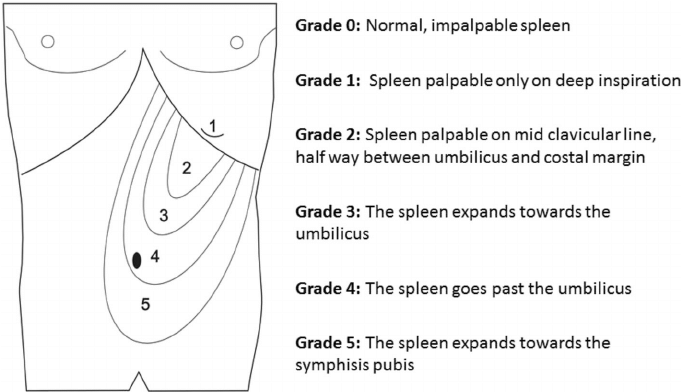
🖼️ Diagram