Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Prostate cancer
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: | Urothelial Tumours | Haematuria | Acute Urinary Retention | Anuria and Oliguria | Bladder Cancer | Renal Cell Carcinoma | Benign Prostatic Hyperplasia | IgA Nephropathy | Prostate Cancer | Henoch-Schonlein Purpura | Glomerulonephritis
🧪 PSA (Prostate-Specific Antigen) is elevated in various prostate diseases. 📈 PSA velocity = rate of PSA change over time. 🦴 PSA >100 ng/mL usually suggests bony involvement. ✋ Rectal exam does not significantly raise PSA. ⚗️ PSA is a 34 kDa glycoprotein protease secreted by epithelial cells of the prostate acini, helping liquefy semen. 🔺 Elevated PSA may reflect prostate cancer, BPH, ageing, post-ejaculation, or prostate calculi.
📌 About Prostate Cancer
- 🧓 Often detected incidentally at post-mortem >70 yrs.
- ⚖️ Main challenge = when to screen and when to treat.
- 🔍 Screening has not consistently shown survival benefit.
- 💉 Cancer growth is testosterone-dependent.
📊 Epidemiology
- 🇬🇧 UK: ~41,700 new cases/year.
- 📉 Only 1% diagnosed <50 yrs.
- 🏿 Higher prevalence in Black African/Caribbean men.
- 👨 Family history ↑ risk ×3.5.
- 🚬 Smoking + ⚖️ obesity linked to more aggressive disease.
🧫 Pathology
- 95% = acinar adenocarcinoma from glandular epithelium.
- 5% = squamous, transitional or rare variants.
- 📍 Most arise in the peripheral zone.
- 🔺 PIN (Prostatic Intraepithelial Neoplasia) = precursor lesion.
- 🧪 PSA + acid phosphatase secreted by prostate epithelium.
🩺 Clinical Presentation
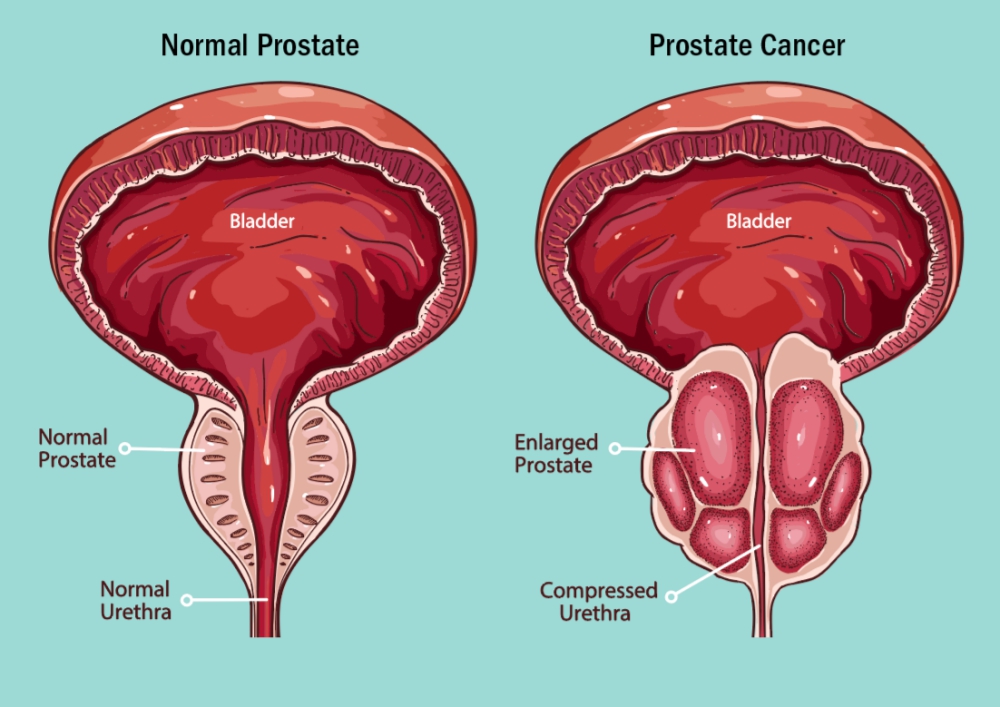
- 💧 LUTS: frequency, nocturia, weak stream, dribbling.
- 🦴 Bone pain or pathological fracture = likely metastasis.
🧩 Common Presentations
- 📈 Raised PSA (screening or post-TURP histology).
- ✋ DRE: hard, craggy prostate, loss of median sulcus.
- 🚽 Outflow obstruction → renal impairment.
- 🦴 Osteosclerotic mets → pain, fracture.
- Advanced: haematuria, haematospermia, obstruction.
📐 PSA Reference Ranges
- 👨 <50 yrs: <3 ng/mL.
- 60–69 yrs: <4 ng/mL.
- >70 yrs: <5 ng/mL.
- <10 ng/mL: usually BPH/prostatitis, but cancer in 20%.
- >10 ng/mL: ~50% chance of malignancy.
🔍 Investigations
- 🩸 U&E: renal function. ALP ↑ with bone mets.
- 📊 FBC: anaemia or leucoerythroblastic picture.
- 📡 mpMRI now first-line before biopsy.
- 🧪 TRUS-guided biopsy if PSA >4 ng/mL.
- 🦴 Bone scan if PSA >20 ng/mL or bone pain.
- 🧬 Gleason score = grade/aggressiveness.
📊 Risk Stratification (Localised Disease)
| Level | PSA | Gleason | Stage |
|---|---|---|---|
| Low | <10 | 6 | T1–T2a |
| Intermediate | 10–20 | 7 | T2b |
| High | >20 | 8–10 | ≥T2c |
🛠️ Prostate Cancer Treatment (UK – NICE NG131, 2021)
📌 Initial Workup
- Risk stratify with D’Amico or NICE criteria.
- Assess Gleason, PSA, MRI staging ± bone scan.
- Histology mandatory before radical Rx.
🏥 Localised Disease (T1–T2, N0, M0)
Low-risk (≤Gleason 6, PSA <10)- 👀 Active surveillance in stable cases.
- Radical prostatectomy or radiotherapy in young/fit men.
- Prostatectomy ± LN dissection OR EBRT ± 3–6 mo ADT.
- 💡 Brachytherapy in select patients.
- EBRT + 2–3 yr ADT = gold standard.
- Surgery only in expert centres.
📍 Locally Advanced (T3–T4, N0, M0)
- EBRT + long-term ADT improves survival.
- Selected surgery in multimodal settings.
🌍 Metastatic Disease (M1)
Hormone-sensitive (mHSPC)- First-line = ADT (LHRH agonist/antagonist).
- + Docetaxel (high-volume) or novel oral (abiraterone, enzalutamide).
- Continue ADT + abiraterone/enzalutamide.
- + Docetaxel or cabazitaxel if progression.
- 🦴 Radium-223 for bone-only mets with pain.
- 🧬 Olaparib for BRCA/HRR mutation-positive cancers.
🤝 Supportive & Palliative Care
- Bone protection: zoledronic acid or denosumab.
- Manage ADT effects: osteoporosis, metabolic syndrome, fatigue.
- 💊 Palliative radiotherapy for bone pain.
🇬🇧 UK-specific Notes
- Follow NICE NG131 (2021).
- MDT discussion mandatory.
- Lifelong PSA follow-up post-treatment.
- ⚖️ Frailty, comorbidities & QoL central to decisions in older patients.
Case 1 – Low-risk, suitable for active surveillance
62-year-old with LUTS and PSA 6.1 µg/L on primary care testing → 2WW referral; DRE benign, MRI PIRADS-3 apex lesion; targeted + systematic biopsies show Gleason 3+3=6 (Grade Group 1) in 2/12 cores, cT1c, PSA density 0.12. MDT counsels active surveillance per NICE: PSA every 3–6 months, repeat MRI at 12 months (earlier if PSA kinetics concerning), re-biopsy if radiological/PSA progression; optimise LUTS, lifestyle, and discuss triggers for definitive therapy.
Case 2 – Unfavourable intermediate risk, radical treatment
68-year-old with new erectile difficulties; PSA 12.8 µg/L, DRE: firm right hemi-gland; mpMRI PIRADS-5 right peripheral zone with possible extracapsular contact; targeted biopsy: Gleason 4+3=7 (Grade Group 3) in multiple cores, cT2b, CT/bone scan negative. MDT offers radical prostatectomy vs external beam radiotherapy + short-course ADT (4–6 months); patient chooses radiotherapy for nerve-sparing avoidance—plan: image-guided hypofractionation with androgen deprivation, then PSA nadir monitoring and management of GU/GI toxicities.
Case 3 – De novo metastatic, systemic therapy
74-year-old presents with back pain and weight loss; PSA 186 µg/L, DRE: hard, irregular prostate; staging shows multiple bone mets and pelvic nodes (M1b). Start androgen deprivation therapy plus treatment intensification (e.g., abiraterone or docetaxel per fitness/IMDC-style risk), early bone support (vitamin D/calcium; consider denosumab/zoledronate if castration-resistant), and analgesic/radiotherapy for painful sites. Discuss local prostate radiotherapy if low metastatic burden per STAMPEDE-aligned practice; monitor PSA, testosterone, symptoms, and metabolic/cardiovascular risks in primary–oncology shared care.