Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Moyamoya disease
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Subarachnoid Haemorrhage |Haemorrhagic stroke
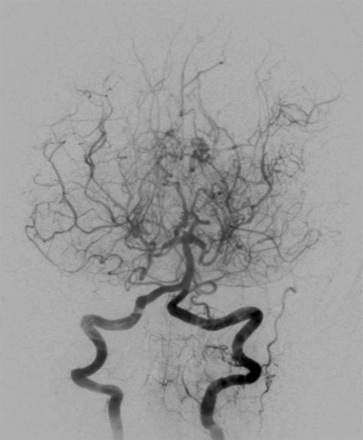
🌫️ Moyamoya disease is a progressive, non-inflammatory vasculopathy affecting the intracranial internal carotid arteries (ICA), middle cerebral arteries (MCA), and anterior cerebral arteries (ACA). It causes both ischaemic and haemorrhagic stroke. On angiography, a hazy network of collateral vessels forms, resembling "moyamoya" — the Japanese word for smoke drifting in the air. First described in 1957, the name was popularised by Jiro Suzuki in 1965 and later codified [Suzuki J, 1983].
📖 About
- Described in Japan in 1957 as “hypoplasia of the bilateral ICAs”; renamed “Moyamoya” in 1965.
- 🧮 Incidence: ~10/100,000 in Japan; ~1/1,000,000 in the USA.
- Involves progressive ICA occlusion and development of fragile collateral vessels.
- Increased basic fibroblast growth factor has been implicated in pathogenesis.
- Can be sporadic or familial, leading to both ischaemic and haemorrhagic stroke.
🧬 Genetics
- Most common in Japanese, Chinese, and Korean populations (10x more frequent than in Europeans).
- Familial clustering: linked to variants on chromosome 17 (e.g., RNF213 gene).
- Seen worldwide, including non-Asian cohorts.
⚙️ Aetiology & Pathophysiology
- Affects the distal ICA, MCA, and ACA stems.
- Results in extensive collateralisation via lenticulostriate, thalamic, and transdural anastomoses.
- Non-inflammatory; pathology shows intimal hyperplasia with lumen narrowing.
- Fragile collaterals predispose to haemorrhage.
- Similar angiographic patterns (“Moyamoya syndrome”) may occur with atherosclerosis, diabetes, or sickle cell disease.
🤝 Associations
- Haematological: Sickle cell disease, β-thalassaemia, hereditary spherocytosis, Fanconi anaemia.
- Neurological/genetic: Neurofibromatosis type 1.
- Metabolic/immune: Homocystinuria, antiphospholipid syndrome, Grave’s disease, SLE.
🩺 Clinical Presentation
- Common in children/young adults, but may present at any age.
- ⛔ Ischaemic events: recurrent hemiplegia, TIAs, cognitive impairment, silent infarcts.
- ⚡ Seizures and movement disorders (chorea, dystonia) may occur.
- 💥 Haemorrhage: intraparenchymal or intraventricular bleed from fragile collaterals.
🔍 Investigations
- 🧪 Bloods: Usually normal; confirms non-inflammatory nature.
- 🖼️ CT: Cortical/subcortical infarcts, volume loss, haemorrhage.
- 🧲 MRI/MRA: Gold standard → ICA narrowing + “puff of smoke” collaterals. FLAIR: “Ivy sign” from slow cortical flow. GRE: Detects microhaemorrhages in basal ganglia/thalamus.
- 📡 Transcranial Doppler: Non-invasive assessment of stenosis/hemodynamics.
- ⚡ EEG: In children → “re-build-up phenomenon” after hyperventilation.
- 🩻 Perfusion imaging: Identifies hypoperfused territories at risk of infarct.
📊 Suzuki Angiographic Stages
- 1️⃣ Early ICA stenosis.
- 2️⃣ Development of Moyamoya collaterals at brain base.
- 3️⃣ Progressive ICA occlusion; ↑ collateral vessels, ↓ MCA/ACA flow.
- 4️⃣ Circle of Willis + PCA occlusion; extracranial–intracranial collateralisation.
- 5️⃣ Fewer Moyamoya vessels; major arteries absent.
- 6️⃣ Disappearance of Moyamoya collaterals; brain perfused only by ECA branches.
⚖️ Management
- Best managed in specialist neurosurgical centres.
- 📉 Medical therapy: Limited role. BP optimisation crucial. Antiplatelets are sometimes used in children but avoided in adults due to haemorrhage risk.
- 🧑⚕️ Surgical revascularisation: - Direct bypass: STA–MCA anastomosis. - Indirect: Encephaloduroarteriosynangiosis (EDAS), burr holes, encephalomyosynangiosis (EMS). Recent studies show direct bypass reduces haemorrhagic risk most effectively.
- 💊 Aspirin often used in children; usually stopped in adults due to bleed risk.
- 📉 Most common cause of death: haemorrhage from fragile collaterals.
📖 Further Reading
- Moyamoya Disease and Syndrome — NEJM, 2009
- Treatment and Outcomes in Moyamoya — J Stroke, 2016
- EEG findings in childhood Moyamoya — Neurosurg Rev, 1992
- MRI vs CT perfusion in Moyamoya — Sichuan Univ J Med, 2018
- Multiple burr hole surgery — Acta Neurochir, 2018
💡 Exam Pearl: Moyamoya = young patient + recurrent TIAs/strokes + angiogram “puff of smoke.” Think early referral for surgical revascularisation to prevent ischaemia and haemorrhage.