Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Normal Pressure Hydrocephalus
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Dementias |Abbreviated Mental Test Score (AMTS) |Alzheimer disease |Dementia with Lewy bodies |Frontotemporal dementia |Corticobasal degeneration |Creutzfeldt Jakob disease |Vascular Dementia |Primary progressive aphasia |Anti Dementia Drugs |AIDS Dementia Complex |Normal Pressure Hydrocephalus |Acetylcholinesterase inhibitors |Mental Capacity Act 2005 |Behavioural and Psychological Symptoms of Dementia
Note: The diagnosis of Normal Pressure Hydrocephalus (NPH) remains controversial ⚖️. Many older adults have gait disturbance, cognitive decline, and ventriculomegaly due to atrophy rather than true NPH. The challenge is identifying those who will genuinely benefit from shunting, as complications are significant.
🌙 About
- NPH is a potentially reversible cause of dementia caused by abnormal CSF accumulation in the ventricles without raised intracranial pressure.
- Classically affects those >60 years old 👴 and was first described by Salomon Hakim in 1965.
- Pathophysiology: Thought to be due to impaired CSF absorption at arachnoid villi → gradual ventricular dilation → compression of periventricular white matter tracts.
⚠️ Causes
- Idiopathic: Majority of cases.
- Secondary: Post-traumatic brain injury, meningitis, subarachnoid haemorrhage (SAH), or tumours obstructing CSF pathways.
🔬 Aetiology
- Disruption of white matter tracts → gait + bladder dysfunction.
- Cortical compression → cognitive slowing and apathy.
- Not fully understood; research into CSF dynamics and glymphatic system is ongoing.
🧩 Clinical Features – Hakim’s Triad
- 🚶♂️ Gait disturbance: “Magnetic gait” (feet stuck to floor), shuffling, difficulty initiating steps.
- 💧 Urinary incontinence: Urgency, frequency, progressing to frank incontinence.
- 🧠 Cognitive decline: Apathy, slowed thought, impaired planning; memory loss less pronounced early on compared to Alzheimer’s.
💡 Mnemonic: "Wet, Wobbly, Wacky" (incontinence, gait, cognition)
🩺 Differential Diagnosis
- Alzheimer’s disease & vascular dementia 🧠
- Parkinson’s disease & atypical parkinsonism 🤚
- Spinal stenosis (gait mimic) 🦴
- Chronic subdural haematoma (exclude with CT/MRI) 💉
📊 Investigations
- Lumbar puncture: Normal opening pressure; large-volume tap (30–40 mL) → transient improvement in gait/cognition suggests shunt responsiveness.
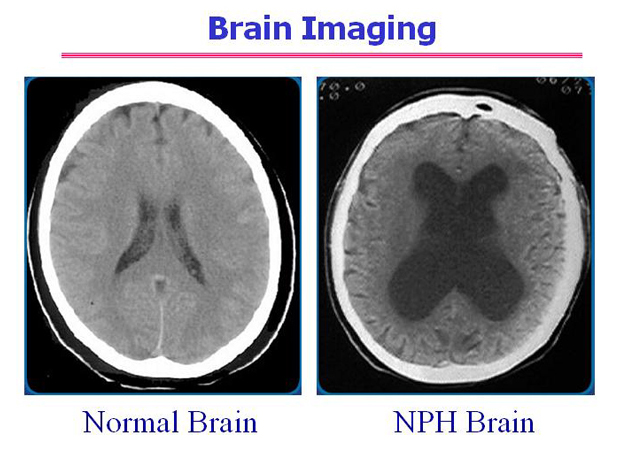
- CT: Ventriculomegaly out of proportion to atrophy (Evans’ index >0.3).
- MRI: Periventricular hyperintensity due to transependymal CSF flow.
- Gait assessment: Before & after LP to assess reversibility.
🖼️ CT scan of NPH
💊 Management
- Pre-shunt testing: LP or external lumbar drainage to select responders.
- Ventriculoperitoneal (VP) shunt: Diverts CSF → peritoneum.
- 🎯 Improvement: 20–90% improve, esp. gait first.
- ⚠️ Complications: infection, bleeding, overdrainage → subdural haematoma.
- Adjustable shunts allow fine-tuning of drainage pressure.
- Conservative: In frail/non-candidates → fall prevention, continence support, therapy.
- Rehabilitation: PT/OT for gait training & ADLs even if shunt is not performed.
📈 Prognosis
- Best outcome if diagnosed early & shunted after positive LP response.
- Gait improves most reliably 🚶♂️, cognition & bladder symptoms less predictable.
- Untreated → progressive disability, dementia, and falls risk.