Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Toxoplasmosis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Herpes Varicella-Zoster (Shingles) Infection |Chickenpox Varicella Infection |Varicella Cerebral Vasculopathy |Herpes Viruses |Herpes Zoster Ophthalmicus (HZO) Shingles |MonkeyPox |Mumps |Measles |Rubella (German Measles) |Epstein-Barr Virus infection |Cytomegalovirus (CMV) infections |CMV retinitis infections |Toxoplasmosis
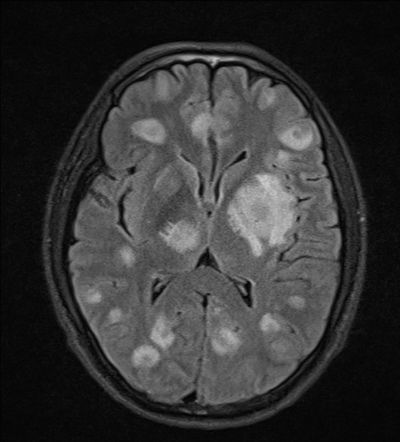
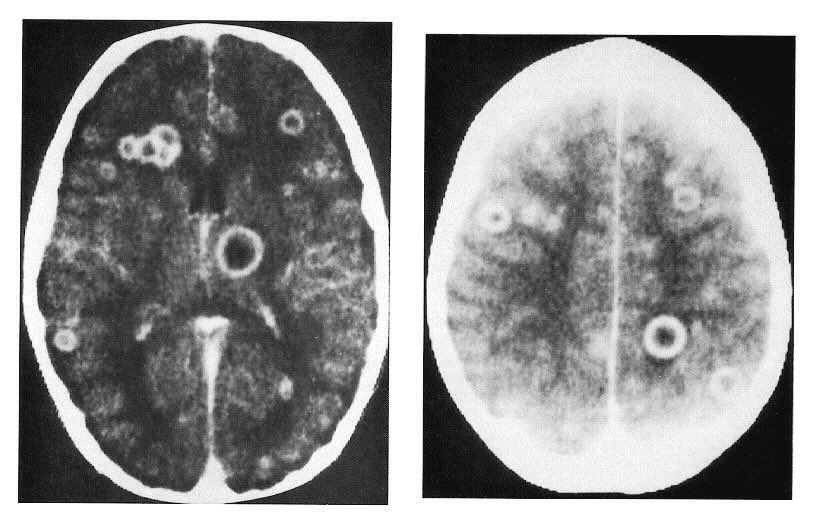
🧠 Causes focal CNS lesions and encephalopathy best seen on MRI, which improve with treatment.
📖 About
- 🦠 Toxoplasmosis is an intracellular protozoan infection caused by Toxoplasma gondii.
- 🇬🇧 About 22% of the UK population are seropositive; 🇫🇷 >90% of the French population are seropositive.
- 🔬 T. gondii was first discovered in 1908 by Charles Nicolle & L. Manceaux in a North African rodent (Ctenodactylus gondii).
🌍 Source
- Foodborne: 🍖 Raw or undercooked meat.
- Zoonotic: 🐱 Cats, 🐦 birds, and contaminated soil.
- Congenital: 👶 Passed from mother to fetus.
- Other: 💉 Blood transfusion.


⚠️ Risks
- 🤰 Pregnancy → high risk to the fetus.
- 🧑⚕️ HIV/AIDS → ~10% of untreated AIDS patients (esp. CD4 <100/mm³).
- 💊 Immunosuppressive therapy → transplant & oncology patients at risk.
🩺 Clinical Presentation (varies with immune status & gestation)
- 🦠 Lymphadenopathy: Cervical nodes, glandular fever–like, often asymptomatic.
- 🧠 Toxoplasmic Encephalitis: Fever, headache, seizures, focal deficits (esp. HIV-positive).
- 👶 Congenital Toxoplasmosis: Microcephaly, hydrocephalus, chorioretinitis, intellectual disability.
- 🌡️ Systemic Toxoplasmosis: Pneumonia, myocarditis, hepatitis (rare if immunocompetent).
- 👁️ Ocular Toxoplasmosis: Retinochoroiditis → eye pain, visual loss.
🔎 Investigations
- Serology: 🧪 Sabin–Feldman test, rising IgG or IgM.
- HIV Testing: Check if immunocompromised.
- Imaging: MRI/CT → multiple ring-enhancing brain lesions (vs single lesion in CNS lymphoma).
- Pulmonary Assessment: CXR/CT for PCP-like pneumonitis.
📑 Diagnostic Criteria
- 🔄 Positive IgG seroconversion.
- 🧪 Specific IgA/IgM + low-avidity IgG (<20%).
- 🧬 Histology: epithelioid cells, follicular hyperplasia.
- 🧫 Parasite detection via PCR or culture.
💊 Management
- 🙂 Asymptomatic (immunocompetent, nonpregnant): No treatment needed.
- 🤒 Symptomatic or Immunocompromised: Sulfadiazine + Pyrimethamine × 6 weeks + MRI monitoring.
- 🧑⚕️ HIV Patients: Start HAART once stable (watch for IRIS).
- 🔍 If no improvement within 3 weeks → reconsider Dx (e.g., CNS lymphoma, tuberculoma).
📚 References
Cases — Toxoplasmosis
- Case 1 — Congenital toxoplasmosis 👶: A 26-year-old woman with cats at home eats undercooked lamb during pregnancy. At 22 weeks, ultrasound shows ventriculomegaly and intracranial calcifications. The newborn has chorioretinitis, hydrocephalus, and seizures. Diagnosis: classic triad of congenital toxoplasmosis. Managed with maternal spiramycin in pregnancy, and pyrimethamine–sulfadiazine plus folinic acid after birth.
- Case 2 — Immunocompromised host 🧬: A 42-year-old man with advanced HIV (CD4 <100) presents with fever, confusion, and focal seizures. MRI brain: multiple ring-enhancing lesions with surrounding oedema. Toxoplasma IgG positive. Diagnosis: cerebral toxoplasmosis. Managed with high-dose pyrimethamine, sulfadiazine, and folinic acid, plus ART optimisation.
- Case 3 — Acquired infection in immunocompetent adult 🥩: A 30-year-old woman presents with low-grade fever, malaise, and cervical lymphadenopathy 2 weeks after eating rare steak. Serology: Toxoplasma IgM positive, IgG rising on repeat. Diagnosis: acquired toxoplasmosis (self-limiting in immunocompetent). Managed with supportive care only.
Teaching Point 🩺: Toxoplasmosis is caused by *Toxoplasma gondii* (cats = definitive host). - In pregnancy: risk of congenital infection → hydrocephalus, intracranial calcifications, chorioretinitis. - In immunocompromised patients: reactivation causes cerebral abscesses. - In healthy adults: often mild, with flu-like illness and lymphadenopathy. Prevention: avoid undercooked meat, wash vegetables, and avoid cat litter in pregnancy.