Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Disseminated Intravascular Coagulation (DIC)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Microangiopathic Haemolytic anaemia |Haemolytic anaemia |Immune (Idiopathic) Thrombocytopenic Purpura (ITP) |Thrombotic Thrombocytopenic purpura (TTP) |Haemolytic Uraemic syndrome (HUS) |Thrombocytopenia |Disseminated Intravascular Coagulation (DIC)
⚠️ Disseminated intravascular coagulation (DIC) is a life-threatening clinicopathological syndrome. It arises from widespread activation of coagulation, generating fibrin clots that cause organ dysfunction, while consuming platelets and clotting factors → paradoxical bleeding + thrombosis. 💀 Classic teaching: “DIC = Death Is Coming”.
📖 About
- Seen in ~1% of inpatients, usually in the context of severe underlying illness.
- Characterised by uncontrolled coagulation → consumption of clotting factors → bleeding.
- Results in massive haemorrhage, microthrombi, multi-organ failure; prognosis is poor.
🦠 Important Causes
- Sepsis – esp. Gram-negative, but also Gram-positive, viral (HIV, CMV, hepatitis), fungal (Histoplasma), parasitic (malaria).
- Trauma & tissue injury – burns, snake bites, crush injuries.
- Malignancy – Acute promyelocytic leukaemia (M3/APL), metastatic cancers.
- Obstetric catastrophes – amniotic fluid embolism, placental abruption, severe pre-eclampsia.
- Other: severe liver failure, transfusion reactions (ABO incompatibility), vasculitis, IBD, aneurysms, recreational drugs.
🧬 Pathophysiology
- Excess thrombin generation → fibrin clots in microvasculature.
- Consumption of fibrinogen & clotting factors.
- Platelet trapping within thrombi → thrombocytopenia.
- Secondary fibrinolysis → ↑ fibrin degradation products (FDPs).
🩺 Clinical Features
- Occurs in critically ill patients.
- Bleeding: IV line sites, surgical wounds, mouth, GI tract, haematuria, epistaxis, intracerebral haemorrhage.
- Microvascular thrombosis → digital ischaemia, organ failure (renal, hepatic, pulmonary, CNS).
- Respiratory failure: ARDS on CXR.
🔬 Investigations
- Platelets: ↓ <50 x10⁹/L.
- PT, APTT, bleeding time: prolonged ⏳.
- Fibrinogen: ↓ <1 g/L.
- Factor VIII, vWF: reduced.
- ↑ FDPs / D-dimer (fibrinolysis markers).
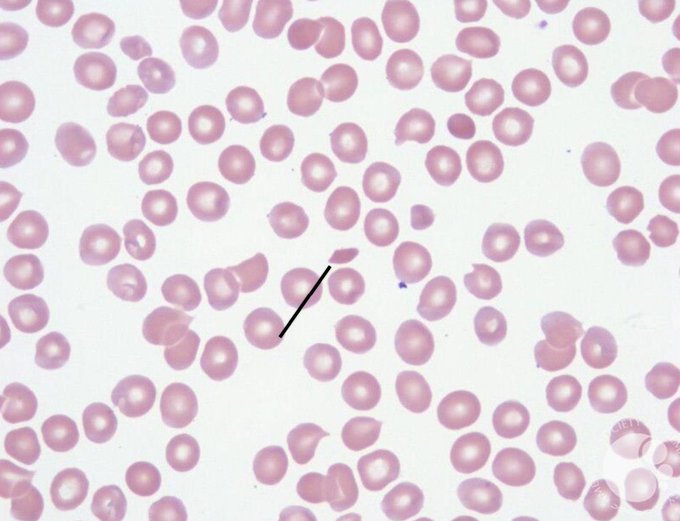
- Blood film: schistocytes (microangiopathic haemolysis).
- CXR: ARDS pattern in severe cases.
📊 Scoring System (Overt DIC – ISTH)
- Platelet count (<100 = 1; <50 = 2).
- Fibrin markers (none = 0; moderate = 2; strong = 3).
- PT prolongation (<3s = 0; 3–6s = 1;>6s = 2).
- Fibrinogen (>1 g/L = 0; <1 g/L = 1).
- Score ≥5 = compatible with overt DIC → repeat daily. <5 = non-overt → repeat every 1–2 days.
📌 Differentials
- Thrombotic thrombocytopenic purpura (TTP).
- Haemolytic uraemic syndrome (HUS).
- HELLP syndrome, pre-eclampsia.
- Severe malignant hypertension.
🩸 Blood Film: Schistocytes
💊 Management (always involve Haematology)
- 1. Treat the underlying cause – sepsis, malignancy, obstetric event, trauma.
- 2. Supportive measures:
- Active bleeding → platelets (<50x10⁹/L) and FFP (15 mL/kg).
- Low fibrinogen (<1 g/L) → cryoprecipitate or fibrinogen concentrate.
- Monitor: platelet count, PT/APTT, fibrinogen after replacement.
- 3. Thrombosis-predominant DIC: therapeutic heparin may be indicated (e.g. purpura fulminans, acral ischaemia).
- 4. Non-bleeding critically ill patients: LMWH prophylaxis to prevent VTE.
- IV Pabrinex if risk of thiamine deficiency in alcoholics/sepsis (avoid precipitating Wernicke’s).
📚 Teaching Pearls
🔑 Think of DIC in any septic, bleeding, or rapidly deteriorating ICU patient. 💡 Labs: low platelets + prolonged PT/APTT + high D-dimer + low fibrinogen = classic pattern. 📉 Prognosis depends on reversing the underlying trigger – supportive therapy alone is insufficient.
📚 Reference
Cases — Disseminated Intravascular Coagulation (DIC)
- Case 1 — Obstetric Emergency: A 32-year-old woman presents with massive postpartum haemorrhage following placental abruption. She is hypotensive and oozing blood from venepuncture sites. Bloods show platelets 45 ×10⁹/L, PT and APTT prolonged, fibrinogen very low, D-dimer markedly elevated. Diagnosis: Acute DIC secondary to obstetric catastrophe.
- Case 2 — Sepsis-Associated DIC: A 70-year-old man with pneumonia becomes hypotensive and develops mottled skin and purpura fulminans. He has active bleeding from his nasogastric tube. FBC: platelets 30 ×10⁹/L, Hb 7.8 g/dL. Coagulation profile: prolonged PT/APTT, low fibrinogen, high fibrin degradation products. Diagnosis: Sepsis-induced DIC.
- Case 3 — Malignancy-Related Chronic DIC: A 65-year-old woman with known metastatic pancreatic cancer presents with bruising, mucosal bleeding, and recurrent venous thromboembolism despite anticoagulation. Platelets are 80 ×10⁹/L, fibrinogen borderline low, PT mildly prolonged, D-dimer persistently elevated. Diagnosis: Chronic DIC in the context of malignancy.
Teaching Commentary 🩸
DIC is a pathological activation of the coagulation cascade, leading to simultaneous thrombosis and bleeding. In the acute setting (e.g., sepsis, trauma, obstetrics), consumption of clotting factors and platelets causes life-threatening bleeding. In chronic forms (e.g., malignancy), the balance is subtler, with recurrent thrombosis alongside bleeding. Diagnosis is clinical plus labs: prolonged PT/APTT, thrombocytopenia, hypofibrinogenaemia, and raised D-dimer. Management focuses on treating the underlying cause, supportive transfusion (platelets, FFP, cryoprecipitate), and careful use of anticoagulation if thrombosis predominates.