Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Subdural haematoma
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Subdural haematoma
🩸 A Subdural Haematoma (SDH) = bleeding between the dura mater and arachnoid.
🧠 Usually venous (bridging veins) → slower onset than extradural bleeds.
⚠️ Classic in the elderly, alcoholics, and anticoagulated patients. Can present acutely (coma) or chronically (confusion, delirium).
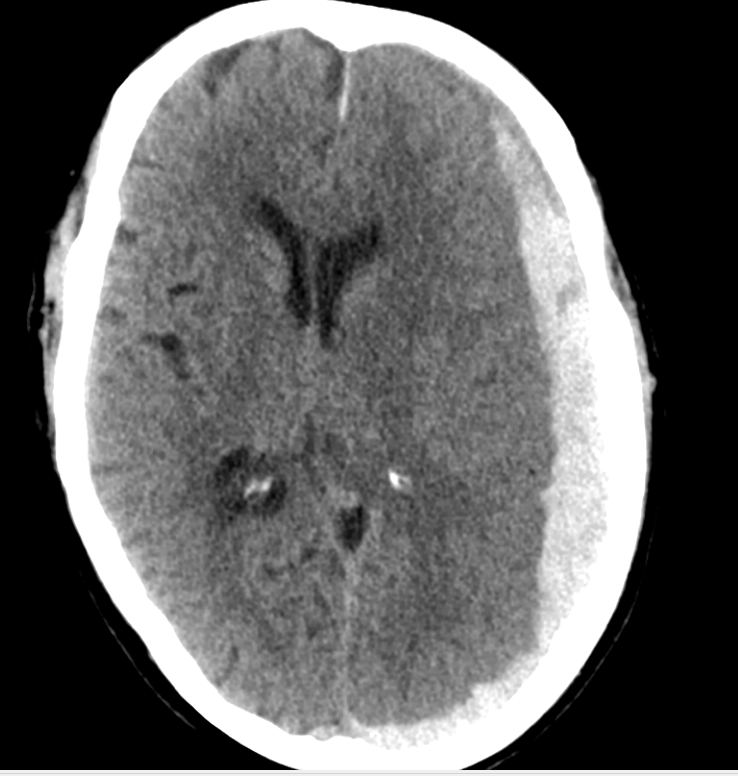
Large Left Subacute SDH with Midline Shift
Large Left Acute SDH with Midline Shift
✅ EDH vs SDH:
- EDH = arterial, biconvex (lens-shaped), does NOT cross sutures, lucid interval.
- SDH = venous, crescent-shaped, CAN cross sutures, insidious/chronic course.
💡 Mechanism
📌 Top Tips
🧬 Aetiology & Causes
🩺 Clinical Features
📷 Imaging Examples

🔬 Investigations
⚠️ Complications
⚡ Management
📋 Key Exam Tips
✅ Think SDH in elderly, alcoholics, or anticoagulated with confusion after a fall.
✅ Always check INR and reverse if anticoagulated.