Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Transverse myelitis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Neurological History taking |Motor Neuron Disease (MND-ALS) |Miller-Fisher syndrome |Guillain Barre Syndrome |Multifocal Motor Neuropathy with Conduction block |Inclusion Body Myositis |Multiple Sclerosis (MS) Demyelination |Transverse myelitis |Acute Disseminated Encephalomyelitis |Cervical spondylosis |Spinal Cord Anatomy |Acute Disc Prolapse |Spinal Cord Compression |Spinal Cord Haematoma |Foix-Alajouanine syndrome |Cauda Equina |Conus Medullaris syndrome |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome
📖 About
- Transverse Myelitis = inflammatory disorder of the spinal cord, affecting grey + white matter and producing motor, sensory, and autonomic dysfunction.
- 🧍♂️ Bimodal distribution: most common in ages 10–20 and >40 years.
- Symptoms vary depending on cord level and whether the lesion is partial or complete.
🔬 Aetiology
- Involves both grey and white matter → wide range of deficits.
- Lesion may be partial (one side/segment) or complete (whole cord cross-section).
🧾 Causes
- ⚡ Autoimmune: MS, ADEM, Neuromyelitis Optica (NMOSD).
- 🌐 Systemic Autoimmune Disease: SLE, Sjögren’s, vasculitis, sarcoid.
- 🦠 Infections: Viral (HIV, EBV, Coxsackie, Zika), Bacterial (Mycoplasma), rare fungal/parasitic.
- 🎗 Paraneoplastic: esp. small-cell lung cancer.
- 💉 Post-vaccination: Rare, causality debated.
⚡ Risk Factors
- Recent infection.
- History of autoimmune disease.
- Genetic predisposition to demyelination.
- Occasional link with recent immunisation.
🩺 Clinical Presentation
- ⏱ Onset: Rapid (hours–days) or subacute (weeks).
- 🌡 Initial: Fever, back pain, myalgia, “band-like” tightness around trunk.
- ⚡ Pain: Often sharp, radiating along dermatomes.
- 💪 Weakness: Spastic paraparesis or quadriparesis.
- 🧊 Sensory loss: Numbness, tingling, loss of pain/temp below level.
- 🚽 Autonomic: Urinary retention, incontinence, constipation.
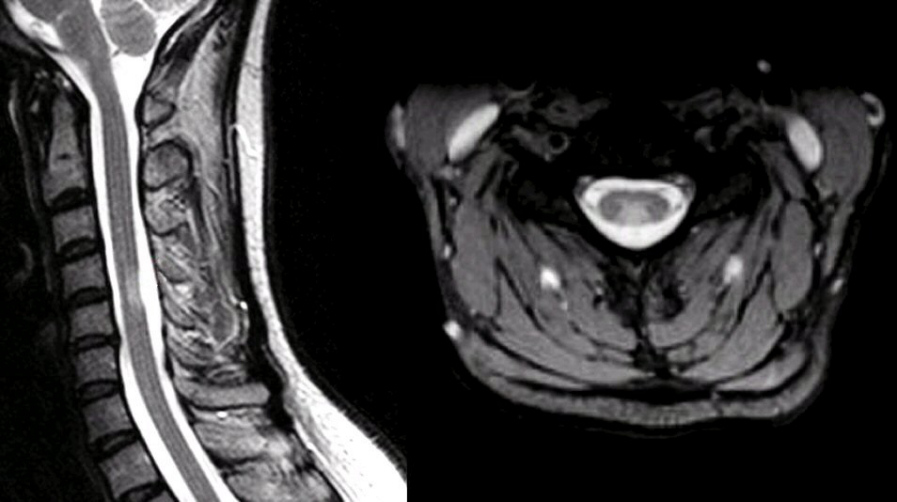
🖼 MRI
🚨 Red Flags
- Sudden severe progression of weakness.
- Respiratory involvement → cervical/high thoracic lesions (can cause ventilatory failure).
- Systemic “B symptoms”: fever, night sweats, weight loss (consider infection/malignancy).
🧪 Investigations
- 🖥 MRI + contrast: Exclude compression, shows T2 hyperintensities spanning ≥3 vertebral segments in NMOSD.
- 💉 CSF: Pleocytosis, raised protein, oligoclonal bands (MS).
- 🧬 Bloods: ANA, ANCA, HIV, EBV, syphilis, aquaporin-4 antibodies (NMOSD).
- ⚡ Evoked Potentials: Detect conduction block in demyelinating disease.
🔍 Differential Diagnosis
- Spinal cord compression (tumour, disc, abscess).
- Multiple sclerosis.
- Spinal cord infarction.
- Neuromyelitis optica spectrum disorder (NMOSD).
- SLE/Sjögren’s-related myelopathy.
💊 Management
- Acute Phase:
- 💉 IV methylprednisolone (3–5 days) → dampens inflammation, improves recovery.
- 🩸 Plasma exchange (PLEX) → for steroid-refractory cases, esp. NMOSD.
- 💉 IVIG → alternative in autoimmune or post-infectious causes.
- Supportive Care: Pain relief, catheterisation, physio, OT.
- Long-term: - Disease-modifying therapy if underlying MS/NMOSD. - Immunosuppression in SLE, Sjögren’s, sarcoid. - Regular rehab to optimise function.
📈 Prognosis
- Variable → some recover fully, others left with deficits.
- Better outcomes with early steroids & limited lesion length.
- NMOSD-related transverse myelitis often severe, relapsing, long cord lesions (“longitudinally extensive TM”).
📝 Exam Pearl: TM = motor + sensory + autonomic dysfunction. Red flag = rapid onset with preserved dorsal column sensation → think infarction instead. Always exclude compressive lesions on MRI before labelling “transverse myelitis.”