Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Aortic Dissection
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Assessing Chest Pain |Acute Coronary Syndrome (ACS) General |Aortic Dissection |Pulmonary Embolism |Acute Pericarditis |Diffuse Oesophageal Spasm |Gastro- oesophageal reflux |Oesophageal Perforation Rupture |Pericardial Effusion Tamponade |Pneumothorax |Tension Pneumothorax |Shingles | Ankle-Brachial pressure Index (ABPI) and Peripheral Vascular Disease | Peripheral Arterial Disease (PAD) | Abdominal Aortic Aneurysm (AAA) | Carotid Endarterectomy | Buerger's disease (Thromboangiitis obliterans ) | Leriche syndrome (aortoiliac occlusive disease)
🚨 The most critical step is to consider aortic dissection in any patient with chest pain — misdiagnosis as MI ❤️🔥 or PE 🩸 is dangerous, since anticoagulation increases the risk of fatal bleeding. Early recognition + urgent referral are lifesaving.
| 🩺 Management of Acute Aortic Dissection |
|---|
|
🤰 Consider dissection in pregnancy and postpartum chest pain (with PE). 🖥️ POCUS can be lifesaving at bedside.
📖 About Aortic Dissection
- Mortality: ~40% die at onset ⚰️; another 10% peri/post-op.
- Urgent CT Aortogram essential 🖥️.
- Type A = surgery; Type B = medical management.
- Beta-blockade crucial to reduce shear stress 💊.
- Chronic dissection (rare) → ongoing pain, HF signs.
🧬 Aetiology
👶 Young patients: connective tissue disorders (e.g. Marfan, Ehlers–Danlos). 👴 Older patients: hypertension, atherosclerosis.
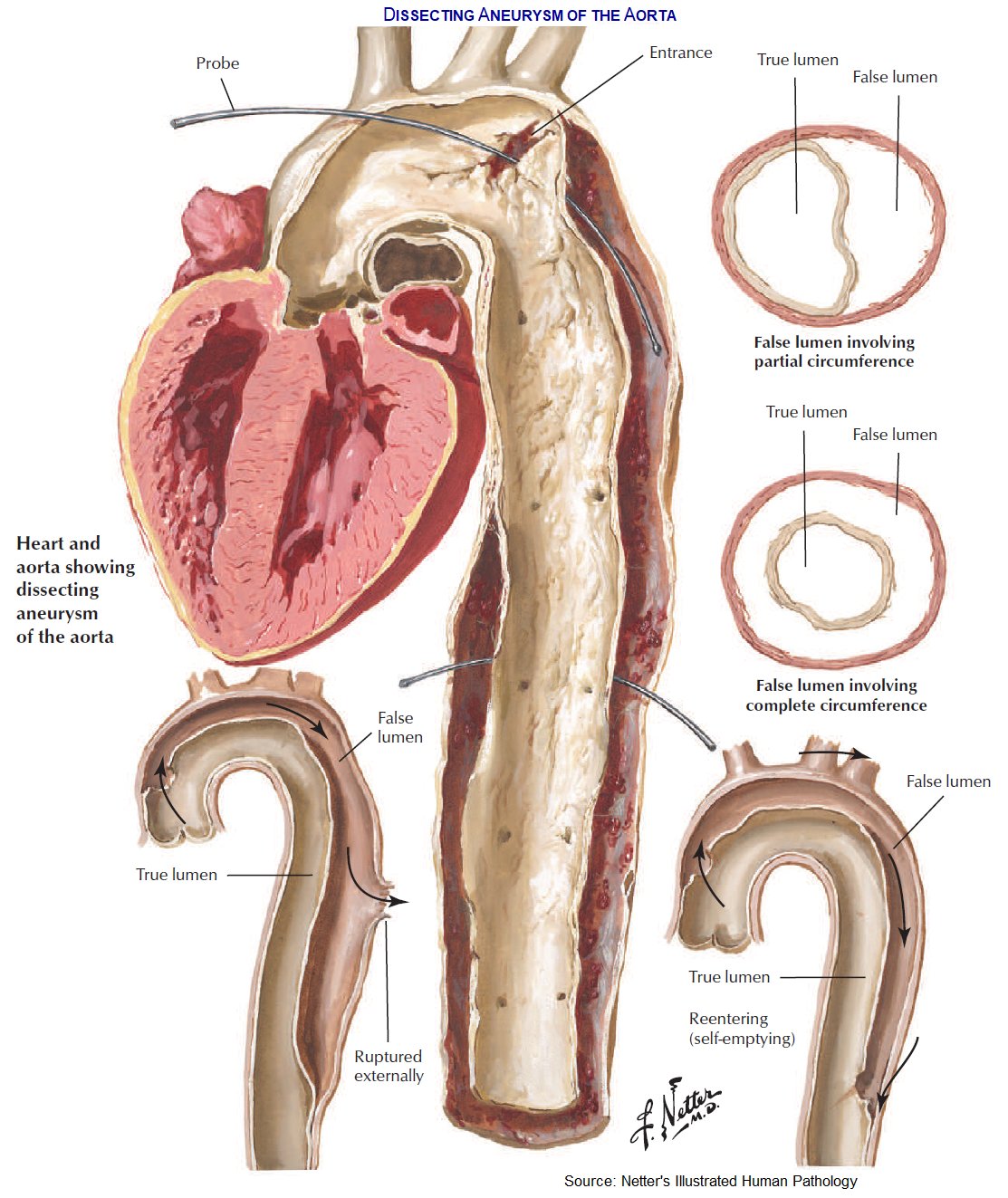
- Aortic wall layers: intima, media, adventitia.
- Tear in intima → blood into media → false lumen forms.
- Extensions: ➡️ Antegrade → distal vessels 🫀 ⬅️ Retrograde → valve, coronaries, tamponade 💧 💥 Rupture → haemothorax, sudden death 🔁 Re-entry → stabilisation possible
 <
<
🗂️ Classification
- Stanford: • Type A = ascending aorta (2/3 cases) ⚡ → surgery • Type B = descending aorta → medical
- DeBakey: • I = Ascending + arch/descending • II = Ascending only • III = Descending only
⚠️ Risk Factors
- ♂ > ♀, >60 yrs
- Hypertension, atherosclerosis
- Connective tissue disorders 🧬
- Trauma, bicuspid AV, prior surgery
- Cocaine use 💊, pregnancy 🤰
- Aortitis (Takayasu, GCA) 🧪
🩺 Clinical Presentation
- Sudden tearing chest pain radiating to back ⚡🖤
- Shock or hypertension, different BP between arms 💪
- Aortic regurg murmur + pulmonary oedema 🌊
- Syncope (~15%) due to tamponade/major vessel occlusion
❗ Complications
- Type A: Tamponade 💧, rupture 💥, AR → HF, stroke 🧠
- Type B: Spinal stroke 🦽, mesenteric/renal ischaemia ⚠️, haemothorax 🫁
🔎 Investigations
- Bloods: U&E, FBC, group & crossmatch 💉
- CXR: widened mediastinum 📏, left pleural effusion
- ECG: may mimic MI (if RCA involved) ❤️🔥
- D-dimer: often ↑, normal helps exclude ❌
- CT Aortogram = gold standard 🖥️
- TOE: rapid diagnosis if unstable
🛠️ Management
- ABC + monitoring ⚡
- Pain: IV morphine 💊
- Lower BP: IV labetalol (± nitroprusside) ⬇️
- Type A = 🚑 surgery (mortality rises 1–2% per hr delay!)
- Type B = strict BP control + endovascular stent (TEVAR) where indicated
📚 References
🧑⚕️ Case Examples — Aortic Dissection
- Case 1 (Type A — ascending aorta): 💔 A 58-year-old man with poorly controlled hypertension presents with sudden severe “tearing” chest pain radiating to the back. He is diaphoretic, with unequal arm BPs. ECG is non-diagnostic, troponin normal. Analysis: Classic Type A dissection involving the ascending aorta — high mortality if untreated. Diagnosis: CT angiography confirms Stanford Type A dissection. Management: Immediate BP control with IV labetalol, urgent cardiothoracic surgical repair.
- Case 2 (Type B — descending aorta): 🫀 A 70-year-old woman with long-standing hypertension and COPD develops sudden tearing interscapular back pain. BP is 210/110, both arms equal. No signs of end-organ malperfusion. Analysis: Stanford Type B dissection (distal to left subclavian artery). Often managed medically if uncomplicated. Diagnosis: CT angiogram shows descending thoracic aortic dissection. Management: Aggressive BP control (IV beta-blocker, vasodilator), pain relief, monitoring. Surgery/endovascular stent reserved for complications (rupture, malperfusion, uncontrolled pain/HTN).
- Case 3 (Complicated dissection with malperfusion): 🚨 A 65-year-old man with Marfan’s syndrome presents with severe chest pain, syncope, and left leg weakness. On exam: BP 90/60, reduced left femoral pulse, new diastolic murmur. Analysis: Aortic dissection complicated by branch vessel involvement (left iliac, aortic regurgitation, possible tamponade). Diagnosis: Stanford Type A dissection with end-organ compromise. Management: Resuscitation, IV beta-blockade, urgent surgical repair. Prognosis poor without immediate intervention.