Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Progressive Supranuclear Palsy (PSP)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: Multiple System Atrophy (MSA) | Parkinson Plus syndromes | Parkinsonism | Idiopathic Parkinson disease | Progressive Supranuclear Palsy | Drug Induced Parkinson disease
Progressive Supranuclear Palsy (PSP) should be suspected in a patient with parkinsonism and early falls. Classic signs include the "Mona Lisa stare" (fixed facial expression, impaired vertical gaze), and MRI findings such as the "Mickey Mouse sign" (axial view) and "Hummingbird sign" (sagittal midbrain atrophy). Early difficulty looking down is a red-flag symptom, as it interferes with reading, eating, and navigating stairs.
About 🧠
- Progressive Supranuclear Palsy (PSP): A rare neurodegenerative disorder, grouped under the atypical parkinsonian syndromes.
- First described by Steele, Richardson, and Olszewski in 1963.
- Classified as a tauopathy, like frontotemporal dementia and corticobasal degeneration.
- Prevalence: ~5–7 per 100,000; mean onset is in the early 60s; male > female.
Etiology & Pathophysiology 🔬
- Caused by abnormal accumulation of 4-repeat tau protein in neurons and glia.
- Predominant involvement of the brainstem (midbrain, pons), basal ganglia, and frontal lobes.
- Severe neuronal loss in the substantia nigra contributes to parkinsonism, but unlike PD, PSP shows poor levodopa responsiveness.
- Frontal cortex and superior colliculus damage explain cognitive slowing and impaired vertical gaze.
Clinical Features 👀🚶
- Early Postural Instability: Recurrent, unexplained backward falls (often the presenting feature).
- Eye Signs:
- Vertical supranuclear gaze palsy (first affects downward gaze).
- Slowed saccades, preserved oculocephalic ("doll's head") reflex.
- "Mona Lisa" / "reptilian" stare: reduced blinking, fixed expression.
- Parkinsonism: Symmetrical, axial rigidity > limb rigidity; bradykinesia with poor levodopa response.
- Other Neurological Signs: Dysarthria, dysphagia, frontal cognitive changes, apathy, pseudobulbar affect.
- Characteristic Posture: Extended neck (retrocollis), unlike flexed posture of PD.
- Dementia: Subcortical type — slowing, impaired executive function, personality change.
Diagnostic Imaging 🖼️
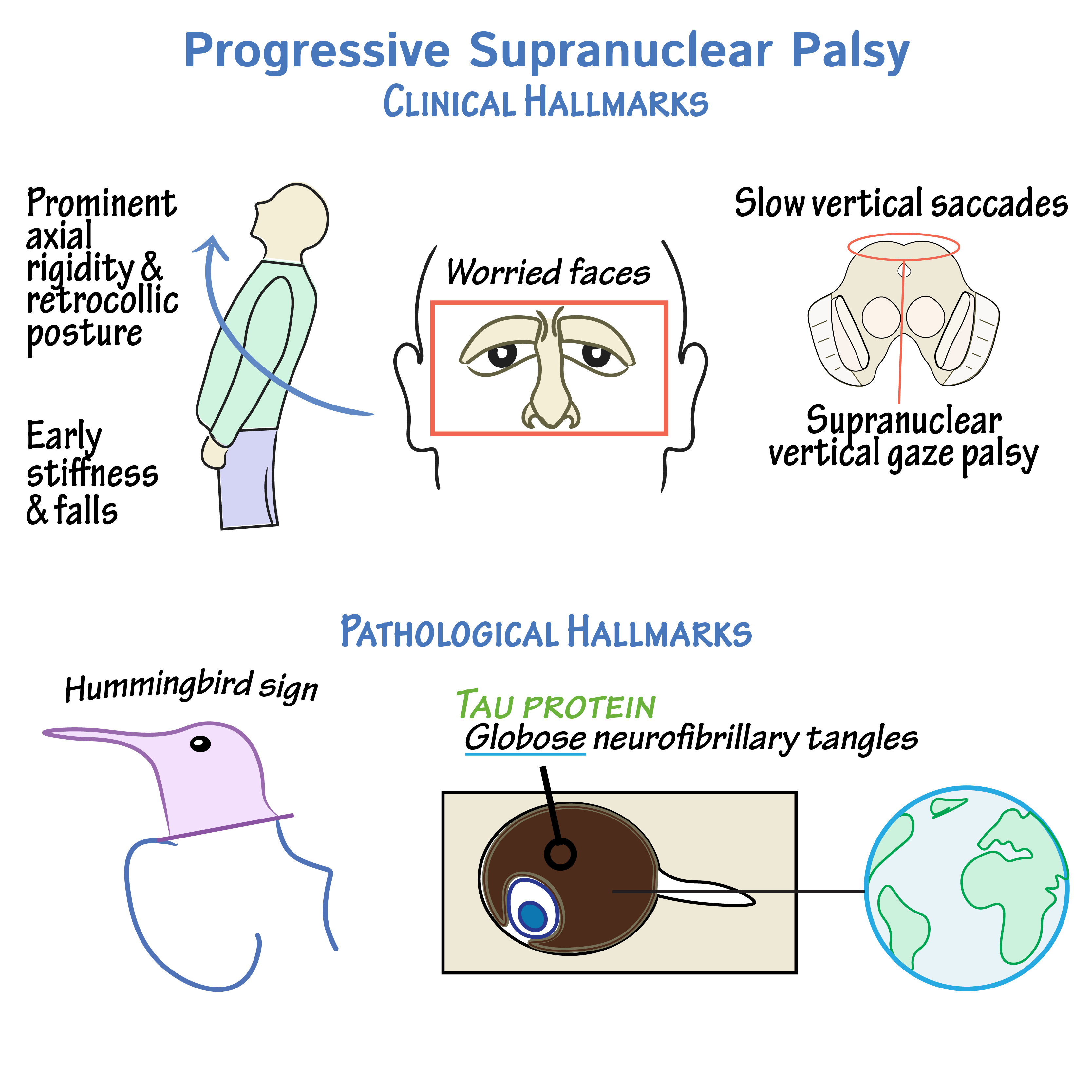
MRI hallmark signs: "Mickey Mouse" midbrain atrophy (axial) and "Hummingbird" sign (sagittal).
Investigations 🔎
- MRI Brain: Midbrain atrophy with preserved pons; hummingbird and Mickey Mouse signs are highly suggestive.
- Neuropsychological Testing: Subcortical dementia pattern (slowed thinking, impaired planning).
- Electrophysiology: Abnormal anal sphincter EMG may support diagnosis.
- Exclusion Work-up: Blood tests to rule out mimics (thyroid disease, Wilson’s, HIV, syphilis).
Differentials ⚖️
- Idiopathic Parkinson’s Disease (PD): Asymmetrical, tremor-dominant, good levodopa response.
- Multiple System Atrophy (MSA): Early autonomic failure, cerebellar features.
- Corticobasal Degeneration (CBD): Asymmetric rigidity, apraxia, cortical sensory loss.
- Frontal-variant Alzheimer’s / FTD: Behavioural change, less parkinsonism.
Management 💊
- Pharmacological:
- Levodopa: Trial recommended, but response usually poor and short-lived.
- Amantadine: May modestly improve gait or fatigue in some patients.
- SSRIs: Useful for apathy, depression, pseudobulbar affect.
- Symptomatic:
- Botulinum toxin: for blepharospasm or dystonia.
- Speech and language therapy: for dysphagia and communication strategies.
- PEG feeding: if aspiration risk becomes high.
- Supportive & Multidisciplinary:
- Physio: balance training, fall prevention, mobility aids.
- OT: home modifications, adaptive equipment.
- Caregiver support and advance care planning are essential.
Prognosis 📉
- Median survival: ~6–8 years after symptom onset.
- Major causes of death: aspiration pneumonia, immobility complications, infections.
- Unlike PD, tremor is rare, and rapid disability occurs due to falls and dysphagia.
OSCE / Exam Tips 🩺
- Clue in Stem: Elderly patient with parkinsonism + early falls + poor levodopa response.
- Look for: Downward gaze palsy, axial rigidity, retrocollis.
- Buzzwords: "Mona Lisa stare," "Hummingbird sign," "Mickey Mouse midbrain."
- Always mention supportive, MDT care — examiners expect it.
References 📚
🧑⚕️ Case Examples — Progressive Supranuclear Palsy (PSP)
- Case 1 (Classic Richardson’s syndrome): 🧑⚕️ A 68-year-old man presents with frequent unexplained falls, difficulty looking down, and progressive stiffness. On exam: vertical gaze palsy (especially downgaze), axial rigidity, and poor postural reflexes. Parkinson’s medications have little benefit. Analysis: Typical PSP presentation — early falls, vertical gaze palsy, poor levodopa response. Diagnosis: Progressive Supranuclear Palsy – Richardson’s phenotype. Management: Supportive care: physiotherapy, occupational therapy, speech therapy, mobility aids. Levodopa trial often ineffective.
- Case 2 (Speech and swallowing predominant): 🗣️ A 72-year-old woman presents with slurred speech, choking on food, and weight loss over 1 year. On exam: spastic dysarthria, slow saccadic eye movements, and early dysphagia. No tremor. Analysis: Bulbar involvement is prominent in some PSP variants. Risk of aspiration pneumonia is high. Diagnosis: PSP with predominant bulbar features. Management: Early referral to speech and language therapy, modified diet, consideration of PEG feeding when aspiration risk rises. Palliative input as disease progresses.
- Case 3 (Frontal variant): 🧠 A 70-year-old retired teacher presents with personality change, apathy, and impaired executive function. Family notes impulsivity and inappropriate jokes. Exam shows mild axial rigidity and limited vertical gaze. Analysis: PSP can mimic frontotemporal dementia when frontal lobe dysfunction dominates, with motor features emerging later. Diagnosis: PSP – frontal variant. Management: Neuropsychiatric support, carer education, community psychiatry involvement. Symptomatic therapies only; disease is relentlessly progressive.