Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Heart and Fetal circulation
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Embryology Heart and Fetal circulation |Embryology Pharyngeal arch derivatives |Embryology of Nervous system |Embryology of Organ Development |Embryology of Blood and Immune System |Embryology of Limb Development
Overview of Heart Development
- The heart develops from mesodermal tissue during early embryogenesis, forming a complex structure that will later provide the foundation for the circulatory system.
- Heart development begins around the third week of gestation and is a highly regulated process involving various signaling pathways and gene expressions.
Stages of Heart Development
- Formation of the Cardiac Tube:
- The heart develops from two endothelial heart tubes that fuse to form a single primitive heart tube.
- This process begins around the 3rd week of embryonic development, shortly after the formation of the mesoderm.
- Looping of the Heart Tube:
- The primitive heart tube undergoes a process called cardiac looping by the end of the 4th week, creating a more complex structure.
- This looping positions the atria and ventricles in their future locations within the heart.
- Chamber Formation:
- During the 5th to 8th weeks, the heart chambers begin to form through the process of septation, which divides the heart into four chambers.
- Septation involves the growth of muscular septa that separate the atria and ventricles and the development of valves.
Key Structures Involved
- Cardiac Jelly: A gelatinous substance that separates the myocardium from the endocardium and plays a role in heart tube formation.
- Myocardium: The muscular layer that forms the walls of the heart and contracts to pump blood.
- Endocardium: The inner layer of endothelial cells that lines the heart chambers.
- Epicardium: The outer layer that also gives rise to coronary blood vessels and contributes to the formation of the heart's pericardium.
Development of Heart Valves
- Heart valves develop from endocardial cushions that form during the process of septation.
- The valves separate the atria from the ventricles (atrioventricular valves) and the ventricles from the great vessels (semilunar valves).
- Proper formation of the valves is crucial for normal heart function, preventing backflow of blood.
Vascular Development
- The heart is connected to a network of blood vessels that develop simultaneously, including the aorta, pulmonary arteries, and veins.
- Formation of the aortic arches occurs, which will later give rise to major arteries in the adult circulatory system.
Clinical Relevance
- Congenital heart defects can arise from errors during the embryonic development of the heart, affecting its structure and function.
- Common congenital heart defects include atrial septal defects, ventricular septal defects, and tetralogy of Fallot, among others.
- Understanding the embryology of the heart is crucial for diagnosing and managing congenital heart diseases and their associated complications.
- Environmental factors, such as maternal diabetes, medications, and alcohol consumption, can influence heart development and increase the risk of congenital defects.
Conclusion
- The embryological development of the heart is a complex process that involves multiple stages and structures, each critical for forming a functional organ.
- Ongoing research continues to explore the genetic and environmental factors that influence heart development and the implications for congenital heart disease.
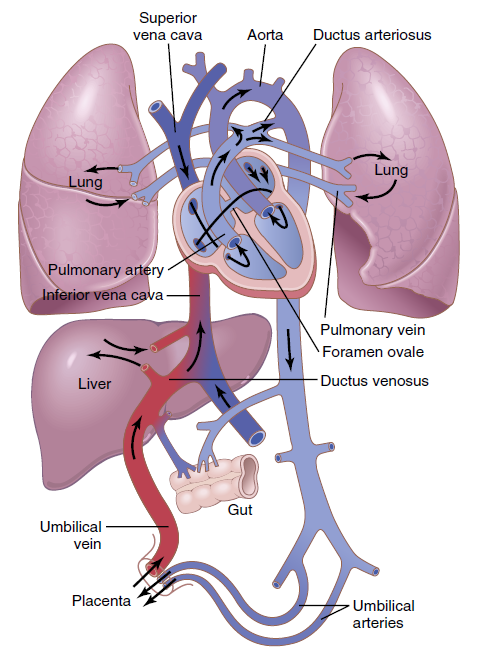
Overview of Fetal Circulation
Fetal circulation refers to the circulatory system of a fetus, which is adapted to support the developing fetus in the womb. The fetus receives oxygen and nutrients from the mother through the placenta, and this system has several unique structures that allow it to function differently from postnatal circulation.
Key Components of Fetal Circulation
- Placenta :
- A complex organ that facilitates the exchange of oxygen, nutrients, and waste products between the maternal and fetal blood.
- The umbilical cord connects the fetus to the placenta, containing two umbilical arteries and one umbilical vein.
- Umbilical Vein :
- Carries oxygenated blood from the placenta to the fetus.
- Half of this blood enters the liver, while the other half bypasses the liver via the ductus venosus, directly entering the inferior vena cava (IVC).
- Ductus Venosus :
- A shunt that allows oxygenated blood from the umbilical vein to bypass the liver and flow directly into the IVC.
- Foramen Ovale :
- An opening between the right and left atria, allowing oxygenated blood to flow from the right atrium to the left atrium, bypassing the lungs.
- Ductus Arteriosus :
- A vessel connecting the pulmonary artery to the descending aorta, allowing most of the blood to bypass the non-functioning fetal lungs.
- Umbilical Arteries :
- Carry deoxygenated blood and waste products from the fetus back to the placenta.
Blood Flow in Fetal Circulation
- Oxygenated blood from the placenta travels through the umbilical vein.
- Blood bypasses the liver via the ductus venosus and enters the IVC, mixing with deoxygenated blood from the lower body.
- The mixed blood enters the right atrium, where it is directed through the foramen ovale to the left atrium.
- From the left atrium, blood flows into the left ventricle and is pumped into the aorta to supply the upper body and brain with oxygen-rich blood.
- Deoxygenated blood returning from the upper body enters the right atrium via the superior vena cava (SVC), flows into the right ventricle, and is pumped into the pulmonary artery.
- Most of the blood in the pulmonary artery bypasses the lungs via the ductus arteriosus, entering the descending aorta.
- Deoxygenated blood is carried by the umbilical arteries back to the placenta for reoxygenation.
Changes at Birth
- At birth, the fetal circulation transitions to the adult circulation pattern:
- The lungs expand and begin to function, increasing blood flow to the lungs.
- The foramen ovale closes as pressure in the left atrium rises above that in the right atrium.
- The ductus arteriosus constricts and eventually becomes the ligamentum arteriosum.
- The umbilical vessels are clamped and cut, and the remnants form ligaments.
Clinical Relevance
- Congenital Heart Defects :
- Abnormalities in the fetal circulation can lead to congenital heart defects, such as patent ductus arteriosus (PDA) and atrial septal defect (ASD).
- PDA: Failure of the ductus arteriosus to close after birth, leading to abnormal blood flow between the aorta and pulmonary artery.
- ASD: Failure of the foramen ovale to close, resulting in a persistent opening between the atria.
- Fetal Monitoring :
- Assessment of fetal circulation is crucial for monitoring fetal health and detecting potential issues.
- Ultrasound and Doppler imaging are commonly used to evaluate blood flow and detect abnormalities.
- Interventions :
- Medical or surgical interventions may be necessary to correct congenital heart defects or manage complications related to fetal circulation.
Summary
Fetal circulation is uniquely adapted to support the developing fetus, with specialized structures that allow the efficient exchange of oxygen and nutrients through the placenta. Understanding the components and pathways of fetal circulation is essential for recognizing normal development and identifying congenital abnormalities. The transition from fetal to postnatal circulation involves significant physiological changes that ensure the newborn's survival and adaptation to life outside the womb.