Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Torsades de pointes TdP (Polymorphic VT)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |ECG-QT interval |Brugada Syndrome |Long QT syndrome (LQTS) Acquired |Long QT syndrome (LQTS) Congenital |Torsades de Pointes |Ventricular Fibrillation |Ventricular Tachycardia |Resuscitation - Adult Tachycardia Algorithm |Automatic Implantable Cardioverter Defibrillator (AICD)
⚡ Torsades de Pointes (Polymorphic VT): Occurs in repetitive, non-sustained paroxysms but can degenerate into VF. 💉 First-line: IV magnesium 8 mmol (2 g) bolus over 10–15 mins in 50–100 ml 5% dextrose or saline. ❌ Avoid amiodarone. Correct K/Mg/Ca. Consider pacing, isoprenaline (except congenital LQTS), and defibrillation if unstable.
📖 About
- Coined by Dessertenne in 1966.
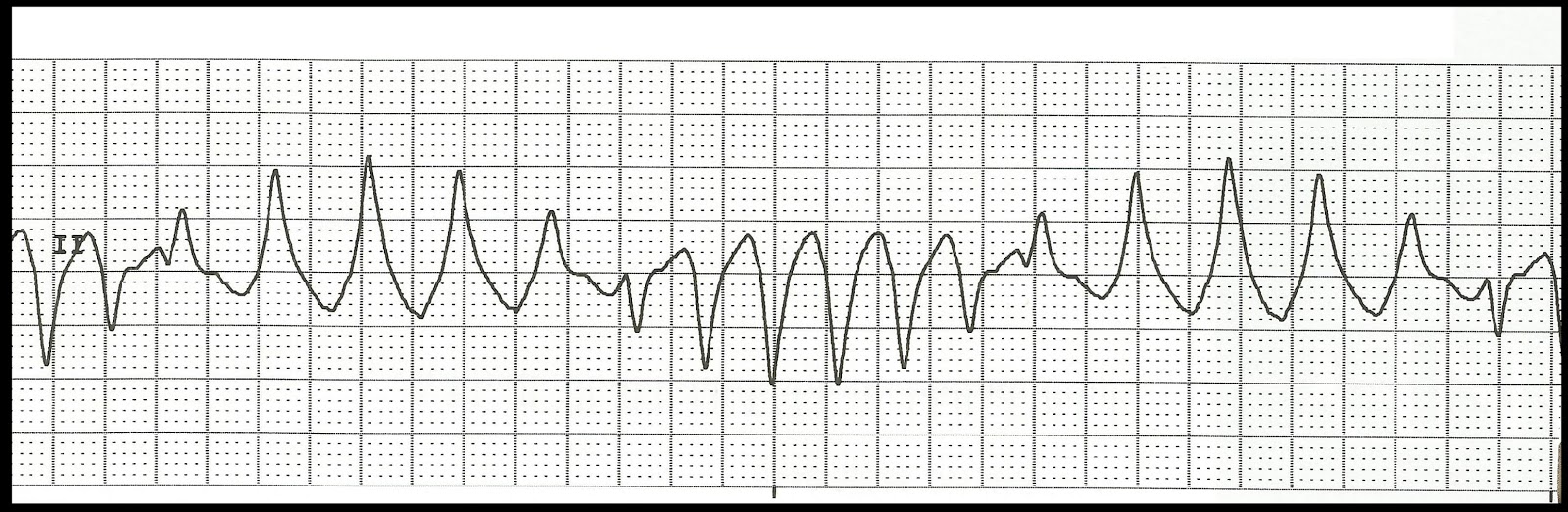
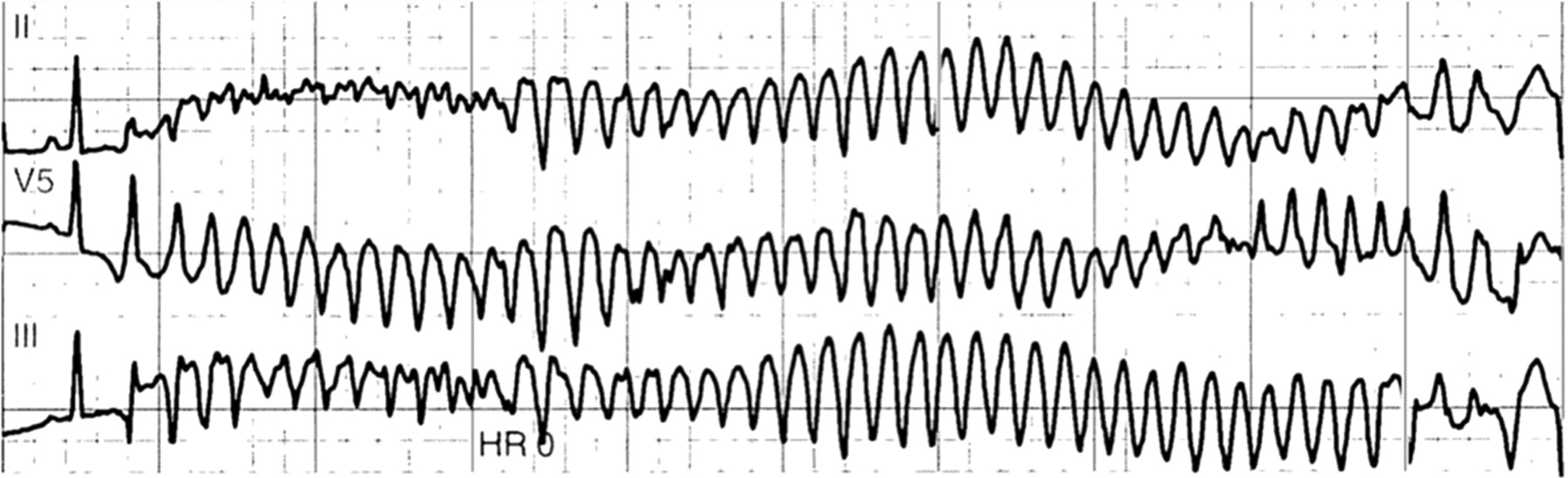
- A polymorphic ventricular tachycardia with the QRS axis “twisting around the baseline.”
- Commonly associated with prolonged QTc >460 ms.
- Drug-associated risk varies — see www.qtdrugs.org.
📌 Definition
- Polymorphic VT with continuously changing QRS axis.
- Seen in congenital or acquired Long QT syndrome.
- Often due to inhibition of the HERG potassium channel.
🖥️ Electrocardiogram
🧬 Genetics
- LQT1 & LQT2 → slow potassium channels.
- LQT3 → sodium channel defects.
- LQT4–12 → rarer subtypes.
- Congenital long QT: autosomal dominant, more pronounced in females.
📊 Epidemiology
- Females 2–3x more likely to develop TdP.
- Drug-induced QT prolongation more common in women.
🩺 Clinical
- Occurs in bursts, often self-terminating.
- Symptoms: presyncope, syncope, hypotension, pulmonary oedema.
- May deteriorate to sustained VT/VF → cardiac arrest.
⚠️ Risk Factors
- Congenital: Romano-Ward (AD), Jervell-Lange-Nielsen (AR + deafness).
- Acquired: electrolyte disorders (↓K, ↓Ca, ↓Mg), medications, bradycardia.
- Other: baseline ECG abnormalities, renal or liver impairment, female sex.
💊 Causes of Acquired Long QT
- Electrolyte/metabolic: hypokalaemia, hypocalcaemia, hypomagnesaemia, hypothyroidism, hypothermia.
- Drugs: amiodarone, disopyramide, flecainide, erythromycin, terfenadine, TCAs, quinidine, lithium, phenothiazines. 👉 Always check in BNF.
🔎 Investigations
- FBC, U&E, Mg, Ca, TFTs, troponin if ACS suspected.
- ECG: twisting QRS, prolonged QTc often >500 ms.
- Echocardiogram: rule out structural heart disease.
🛠️ Management
- Stop offending drugs (esp. amiodarone, class I/III antiarrhythmics).
- IV magnesium sulphate: 8 mmol (2 g) bolus → then 72 mmol (18 g) over 24 hrs.
- Pacing (atrial > ventricular) if bradycardia-dependent TdP.
- IV isoprenaline: useful for acquired TdP but contraindicated in congenital LQTS.
- Defibrillation if unstable.
- Congenital LQTS: beta-blockers mainstay; consider ICD or left stellate ganglion block for refractory cases.
- Acquired LQTS: beta-blockers contraindicated (bradycardia worsens risk).
📚 References
💡 Teaching Pearl: TdP is always a “red flag rhythm.” Think: correct electrolytes, stop QT-prolonging drugs, give magnesium, pace or shock if needed.