Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Cushing syndrome
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
⚠️ Important: Hypokalaemia is more likely when the source of ACTH is malignant. 🧠 A normal pituitary MRI does not exclude Cushing’s disease – up to 50% (especially children) may have normal imaging. 👉 In such cases, inferior petrosal sinus sampling is crucial.
📖 About
- Cushing's Syndrome = chronic exposure to excessive cortisol.
- Disrupts hypothalamic–pituitary–adrenal (HPA) axis feedback 🔄.
- Loss of normal circadian cortisol rhythm 🌙☀️.
- Cushing’s Disease = pituitary adenoma secreting ACTH.
🧬 Aetiology
- 🌟 ACTH-dependent:
- 🧠 Pituitary adenoma (Cushing’s disease).
- 🫁 Ectopic ACTH from tumours (e.g. lung, pancreas).
- 🌟 ACTH-independent:
- 🟤 Adrenal adenomas/carcinomas.
- 💊 Exogenous glucocorticoids (most common overall cause).
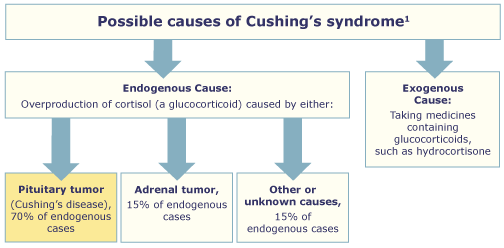
⚡ Causes
- 🧠 Pituitary Adenoma (Cushing’s Disease) (~70% endogenous)
- Microadenomas → ↑ACTH → bilateral adrenal hyperplasia.
- Key: not suppressed by low-dose dex, partially suppressed by high-dose; ↑ACTH & cortisol; responds to CRH.
- 🟤 Adrenal Tumours
- Autonomous cortisol secretion → suppressed ACTH.
- No suppression on low or high-dose dex.
- 🫁 Ectopic ACTH Production
- Sources: small cell lung carcinoma, bronchial carcinoid, pancreatic NET.
- ACTH high, no suppression on high-dose dex.
- Often severe hypokalaemia ⚠️ due to mineralocorticoid activity.
- 💊 Iatrogenic – long-term glucocorticoid therapy (asthma, RA, PMR, UC, post-transplant).
- 🎭 Pseudo-Cushing’s – alcohol excess, severe obesity, depression (reversible).
- 🤰 Pregnancy – ↑ cortisol-binding globulin → raised total cortisol (rarely true Cushing’s).
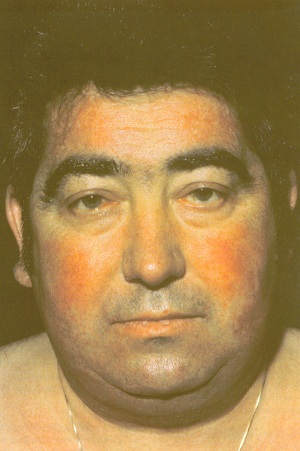
👀 Clinical Features
- Appearance 🌙:
- Centripetal obesity.
- Moon face, facial plethora, acne.
- Dorsocervical fat pad (“buffalo hump”).
- Muscle wasting → thin extremities.
- Purple striae (abdomen, thighs, breasts).
- Skin 🩹:
- Thin fragile skin, easy bruising.
- Slow wound healing.
- Hirsutism in women.
- Hyperpigmentation (if ACTH-driven).
- MSK 💪:
- Proximal myopathy (difficulty standing/climbing stairs).
- Osteoporosis → fractures.
- Avascular necrosis of femoral head.
- Metabolic 🧪:
- Glucose intolerance / diabetes.
- Hyperlipidaemia.
- Hypertension.
- Hypokalaemia & metabolic alkalosis.
- Neuropsychiatric 🧠:
- Mood swings, depression, psychosis.
- Cognitive impairment.
- Reproductive ❤️:
- Women: amenorrhoea, infertility.
- Men: ↓ libido, impotence.
- Growth 📏:
- Stunted growth in children.
- Immune 🛡️:
- Infections, reactivation of TB.
- Poor wound healing.


🧪 Diagnostic Tests
🌙 Overnight Dexamethasone Suppression (screen)
- 1 mg dex at midnight → cortisol at 08:00.
- Normal < 50 nmol/L;> 50 → suspect Cushing’s.
- ⚠️ False positives: depression, obesity, alcohol, phenytoin.
🧪 24h Urinary Free Cortisol (screen)
- Normal < 280 nmol/24h; elevated = abnormal.
💉 Low-Dose 48h Dex Test (confirm)
- 0.5 mg dex 6-hourly × 48h (total 4 mg).
- Cortisol undetectable = excludes; detectable = Cushing’s confirmed.
📊 High-Dose 48h Dex Test (localise)
- 2 mg dex 6-hourly × 48h (total 16 mg).
- Pituitary: >50% suppression.
- Ectopic/adrenal: no suppression.
🧬 Plasma ACTH
- ⬇️ Undetectable → adrenal tumour.
- ⬆️ High → pituitary vs ectopic.
- CRH test: rise = pituitary; no rise = ectopic.
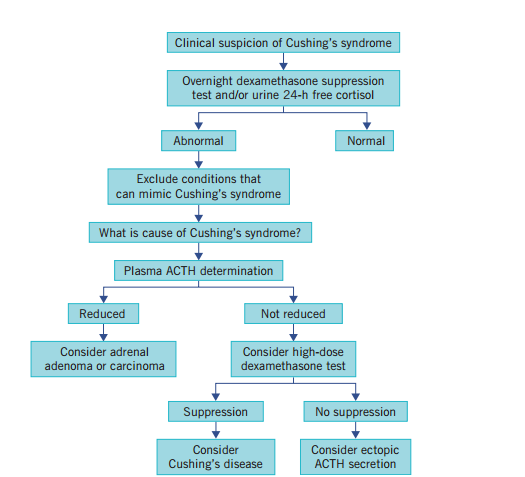
📚 Exam Tip: Think stepwise → Overnight (screen) → Low-dose (confirm) → High-dose/ACTH (localise). Pituitary = suppressible, ectopic/adrenal = resistant.
🖼️ Imaging
- 🧠 Pituitary MRI (but 50% normal!) → may need inferior petrosal sinus sampling.
- 🟤 Adrenal CT/MRI → adenoma or carcinoma.
- 🫁 Chest/abdomen CT → ectopic ACTH tumours.
- 📡 Octreotide scans for ectopic localisation.
💊 Management
- 🧠 Pituitary adenoma: transsphenoidal resection; radiotherapy if unsuccessful; pasireotide or ketoconazole if refractory.
- 🟤 Adrenal tumours: adrenalectomy ± mitotane if carcinoma.
- 🫁 Ectopic ACTH: treat primary tumour if resectable; otherwise medical control of cortisol.
- 💊 Iatrogenic: gradual steroid taper, switch to steroid-sparing alternatives.
🧪 Medical Therapy (for inoperable / pre-surgery)
- Metyrapone (11β-hydroxylase inhibitor).
- Ketoconazole (blocks steroidogenesis).
- Aminoglutethimide (cholesterol → pregnenolone block).
- Mitotane (adrenolytic, carcinomas).
- Etomidate (IV emergency use).
📌 Key Points
- Early recognition prevents morbidity & mortality.
- Diagnosis = stepwise biochemical + imaging + sometimes petrosal sampling.
- Management is cause-directed (surgery first-line where possible).
- 🏥 Long-term follow-up essential: recurrence, metabolic complications, bone health, psychological support.
Cases — Cushing’s Syndrome
- Case 1 — Iatrogenic steroid use 💊: A 55-year-old woman with rheumatoid arthritis on long-term prednisolone presents with weight gain, easy bruising, proximal muscle weakness, and thin skin. Exam: moon facies, buffalo hump, purple abdominal striae. Diagnosis: exogenous Cushing’s syndrome due to chronic glucocorticoid therapy. Managed by gradual tapering of steroids and use of steroid-sparing agents.
- Case 2 — Pituitary-dependent (Cushing’s disease) 🧠: A 36-year-old woman presents with irregular menses, hirsutism, and worsening acne. Exam: central obesity, hypertension, and skin thinning. Bloods: elevated cortisol not suppressed by low-dose dexamethasone, but suppressed with high-dose dexamethasone. MRI: pituitary microadenoma. Diagnosis: Cushing’s disease (ACTH-secreting pituitary adenoma). Managed with trans-sphenoidal pituitary surgery.
- Case 3 — Adrenal tumour ⚠️: A 42-year-old man presents with new-onset diabetes, hypertension, and muscle wasting. No exogenous steroid use. Bloods: raised cortisol with suppressed ACTH. CT abdomen: adrenal mass. Diagnosis: ACTH-independent Cushing’s syndrome due to adrenal adenoma. Managed with adrenalectomy.
Teaching Point 🩺: Cushing’s syndrome = chronic glucocorticoid excess. Common causes: exogenous steroids, pituitary adenoma (Cushing’s disease), adrenal adenoma/carcinoma, ectopic ACTH (e.g. small-cell lung cancer). Clinical clues: central obesity, moon facies, striae, proximal weakness, hypertension, diabetes, mood changes. Diagnosis: screen with 24h urinary cortisol, overnight dexamethasone suppression, late-night salivary cortisol. Management: treat underlying cause (taper steroids, pituitary surgery, adrenalectomy).