Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Idiopathic Intracranial hypertension
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Brain tumour s |Astrocytomas |Brain Metastases |Tuberous sclerosis |Turcot's syndrome |Lhermitte Duclos Disease |Oligodendroglioma |Acute Hydrocephalus |Intracranial Hypertension |Primary CNS Lymphoma (PCNSL)
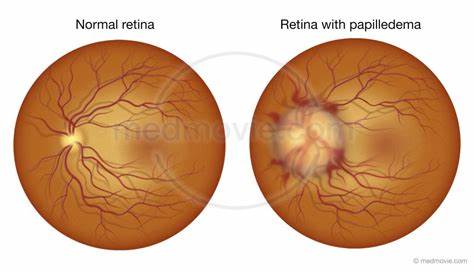
👩⚕️ Idiopathic Intracranial Hypertension (IIH), also called Pseudotumour Cerebri, is a syndrome of raised intracranial pressure without an identifiable structural cause. ⚠️ Though “benign” in name, it is not harmless — untreated, it may cause permanent visual loss from papilloedema.
ℹ️ About
- Most common in young, obese females 📈.
- Mimics a brain tumour clinically and radiologically (hence “pseudotumour”).
- Visual field defects (early blind spot enlargement, inferonasal loss) are characteristic. 👁️
🧬 Aetiology
- Exact cause unknown, but linked to impaired CSF absorption at arachnoid granulations.
- Cerebral venous sinus thrombosis must always be excluded. 🚨
🤝 Associations
- Pregnancy, OCP use, thrombophilia.
- Drugs 💊: Vitamin A/retinoids, tetracyclines (minocycline, doxycycline), growth hormone, nitrofurantoin, danazol, lithium.
- Others: Ketamine, nitrous oxide.
🩺 Clinical Presentation
- Headache: Morning-predominant, worse lying down, eased by ICP reduction.
- Visual: Transient obscurations, blurred vision, papilloedema, visual field loss.
- Other: Diplopia (CN VI palsy), pulsatile tinnitus, neck/back pain.
- Often history of recent weight gain ⚖️ or new medication exposure.
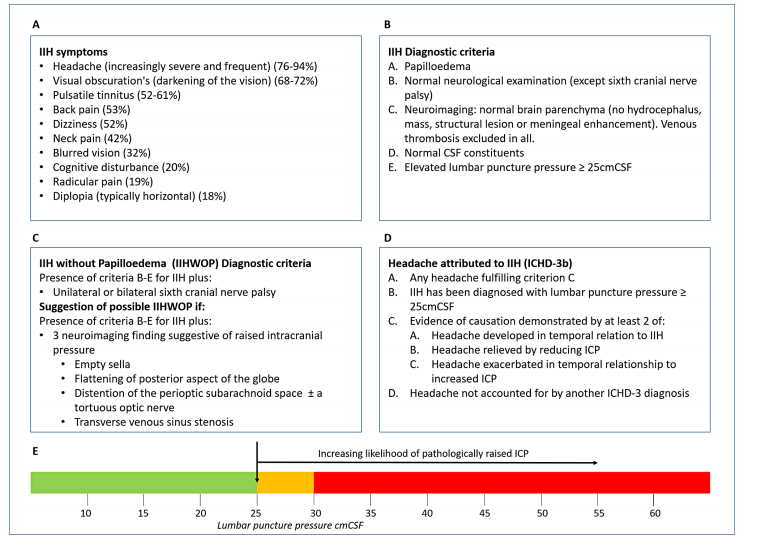
🔬 Investigations
- Bloods: FBC, U&E, LFT, ESR, CRP to exclude systemic causes.
- Visual field testing: Blind spot enlargement, inferonasal defects.
- Imaging: MRI/MRV to exclude mass or venous thrombosis; may show empty sella, enlarged optic nerve sheath.
- LP: Elevated opening pressure (>25 cm H₂O) with normal CSF constituents.
📑 Diagnostic Criteria (Modified Dandy Criteria)
|
🧾 Differentials
- Cerebral venous sinus thrombosis
- Intracranial mass lesion (tumour, abscess)
- Hydrocephalus
🎯 Management Goals
- Rule out venous sinus thrombosis.
- Preserve vision 👁️.
- Reduce ICP and control headache burden.
💊 Management
- Stop offending drugs (e.g., tetracyclines, retinoids, steroids, nitrofurantoin).
- Weight loss: 5–10% reduction can significantly lower ICP; bariatric surgery may be considered.
- Medical therapy:
- Acetazolamide (carbonic anhydrase inhibitor) — first-line; reduces CSF production.
- Topiramate — useful alternative (also promotes weight loss).
- Loop diuretics (e.g., furosemide) in selected cases.
- Steroids rarely used — rebound ICP rise on withdrawal.
- Surgical options:
- Optic nerve sheath fenestration — for threatened vision, rapidly reduces papilloedema.
- CSF diversion (VP or LP shunt) — in refractory disease.
- Venous sinus stenting — emerging therapy for stenosis-related IIH.
💡 Exam Pearl
Think “young obese woman with headache + papilloedema + raised LP opening pressure.” 👉 Always exclude venous sinus thrombosis before labelling as IIH. 👉 First-line treatment = weight loss + acetazolamide.