Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Colposcopy
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Causes of abnormal Vaginal bleeding |Vaginal Carcinoma |Cervical cancer |Endometrial (Uterine) Cancer |Post Menopausal Bleeding |Anatomy of the Uterus |Anatomy of the Ovary |Gynaecological History Taking |Colposcopy |Premature Menopause |Polycystic Ovary syndrome
Colposcopy
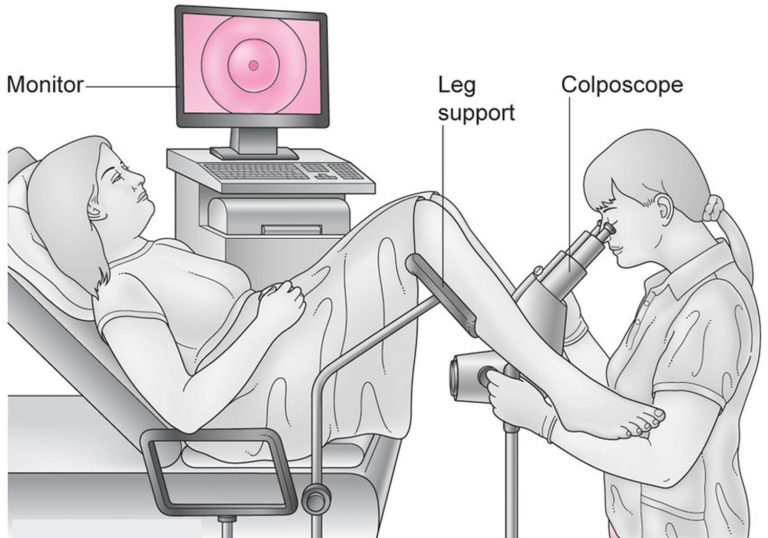
Colposcopy is a specialized diagnostic procedure employed in the evaluation of cervical, vaginal, and vulvar pathology. By using a colposcope—an instrument that provides magnified and illuminated visualization—clinicians are able to detect subtle epithelial changes that may indicate dysplasia or early neoplastic transformation. This article outlines the key aspects of colposcopic practice, including indications, equipment, procedural technique, and post-procedure management.
Indications
- Abnormal Cervical Screening: Colposcopy is primarily indicated following abnormal Pap smear findings (e.g., ASC-US, LSIL, HSIL) and/or positive high-risk HPV tests.
- Visible Cervical Abnormalities: When an abnormal cervical appearance is noted during a pelvic examination, colposcopy can help localize lesions.
- Post-Treatment Surveillance: Follow-up evaluation after excisional or ablative therapy for cervical intraepithelial neoplasia (CIN) is performed to assess treatment efficacy and detect residual or recurrent disease.
- Other Clinical Scenarios: Colposcopy may also be used to investigate unexplained vaginal or postcoital bleeding, or in cases of suspected cervical adenocarcinoma in situ.
Equipment and Personnel
Successful colposcopic evaluation relies on proper equipment and trained personnel. Essential equipment includes:
- Colposcope: A binocular microscope with adjustable magnification (typically ranging from 2× to 25×) and an integrated light source, often equipped with red-free filters to enhance visualization of vascular patterns.
- Specula: A range of vaginal specula (metal or plastic) are used to retract the vaginal walls and expose the cervix.
- Solutions: Acetic acid (usually 3-5%) is applied to highlight acetowhite changes; Lugol’s iodine may also be used (Schiller test) to distinguish glycogen-rich normal epithelium from dysplastic areas.
- Biopsy Instruments: Punch biopsy forceps, endocervical brushes or curettes are required for tissue sampling from suspicious areas.
In addition to the colposcopist, a well-trained assistant is recommended to handle instruments and document findings. A chaperone should also be present to ensure patient comfort and safety.
Procedure Technique
Colposcopy is performed in an outpatient setting, typically following these steps:
- Patient Preparation: The patient is positioned in the dorsal lithotomy position. A detailed medical history is obtained, and informed consent is secured.
- Speculum Insertion: A speculum is inserted to expose the cervix and adjacent vaginal walls.
- Initial Visual Examination: Under low magnification, the colposcopist evaluates the overall architecture and identifies the squamocolumnar junction and transformation zone.
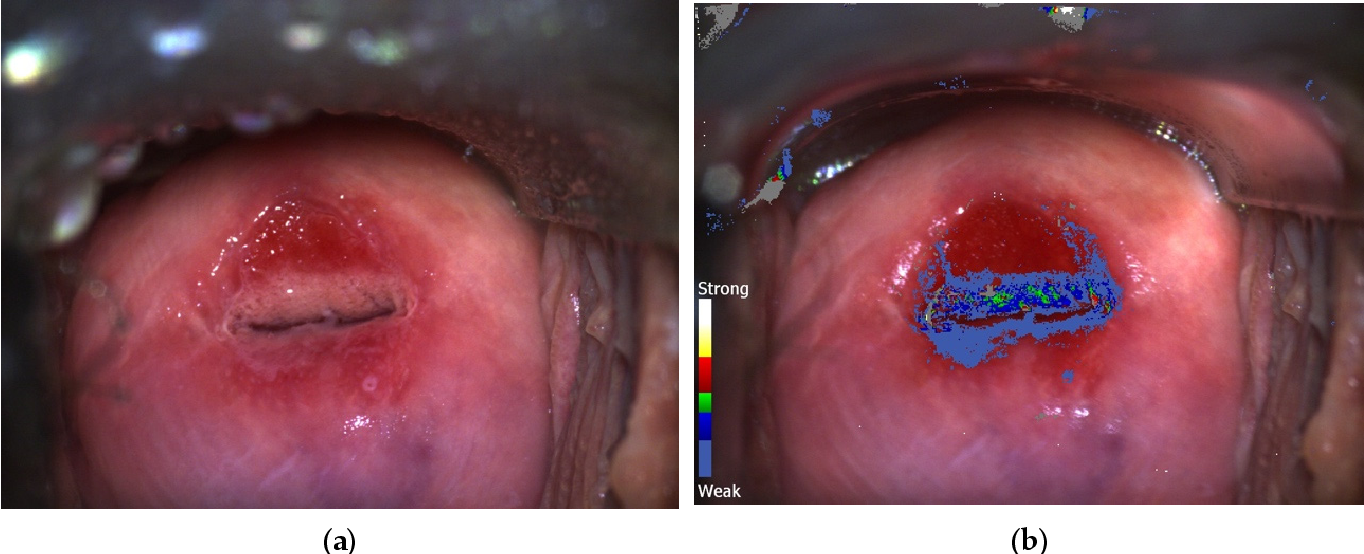
- Application of Acetic Acid: A cotton swab soaked in acetic acid is applied to the cervix. Abnormal epithelial areas typically turn white (acetowhitening), accentuating lesion borders and vascular patterns.
- Application of Lugol’s Iodine (Optional): Iodine solution may be applied to further differentiate normal from abnormal tissues; normal cells stain brown while dysplastic areas remain unstained or appear yellow.
- Documentation and Biopsy: Detailed observations, including lesion size, margins, and vascular changes, are documented. Targeted biopsies are taken from any areas exhibiting significant abnormalities. If necessary, an endocervical sampling is performed when the transformation zone is not fully visible.
Complications and Pitfalls
- Procedural Risks: Although colposcopy is generally safe, potential complications include minor bleeding, infection, and patient discomfort, particularly following biopsy.
- Visualization Challenges: Incomplete visualization of the transformation zone—due to anatomical variations or scarring—may limit diagnostic accuracy. In such cases, supplementary procedures such as endocervical curettage are indicated.
- Interobserver Variability: There is recognized variability in colposcopic impressions among practitioners, which underscores the importance of standardized guidelines and ongoing training.
Follow-Up and Management
Following the colposcopic examination, biopsy specimens are processed and analyzed by a pathologist. The results guide further management:
- Normal Findings: Routine screening and follow-up are continued as per guidelines.
- Low-Grade Lesions: Patients may be managed with observation and repeat cytology, with colposcopy reserved for persistent abnormalities.
- High-Grade Lesions: These typically necessitate excisional treatment (e.g., LEEP or cone biopsy) and close surveillance.
Conclusion
Colposcopy remains an indispensable diagnostic tool in the prevention and early detection of cervical cancer. By enabling magnified visualization of the cervix and allowing for targeted tissue sampling, colposcopy aids clinicians in accurately diagnosing cervical dysplasia and planning appropriate treatment. Adherence to standardized procedures and guidelines, along with continuous training, are essential for maintaining high diagnostic accuracy and improving patient outcomes.