Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Diabetes: Eye Disease
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: Type 1 DM |Type 2 DM |Diabetes in Pregnancy |HbA1c |Diabetic Ketoacidosis (DKA) Adults |Hyperglycaemic Hyperosmolar State (HHS) |Diabetic Nephropathy |Diabetic Retinopathy |Diabetic Neuropathy |Diabetic Amyotrophy |Maturity Onset Diabetes of the Young (MODY)
👁️ Diabetic retinopathy is largely preventable: tight glycaemic control, BP and lipids slow microvascular damage; timely laser/anti-VEGF preserves sight. In the UK, routine annual screening from age 12 (NHS DES) catches asymptomatic disease early.
📖 About
- ~50% of T1D affected within 10–15 years; ~50% of T2D within 15 years. Most changes are mild if detected early.
- Risk rises with diabetes duration, hyperglycaemia (HbA1c), hypertension, dyslipidaemia, nephropathy, pregnancy, and smoking.
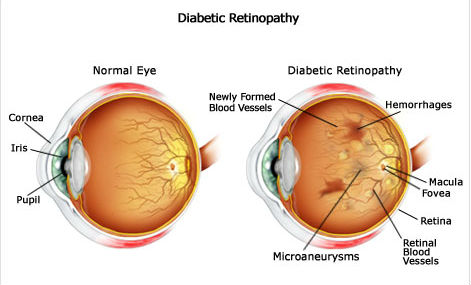
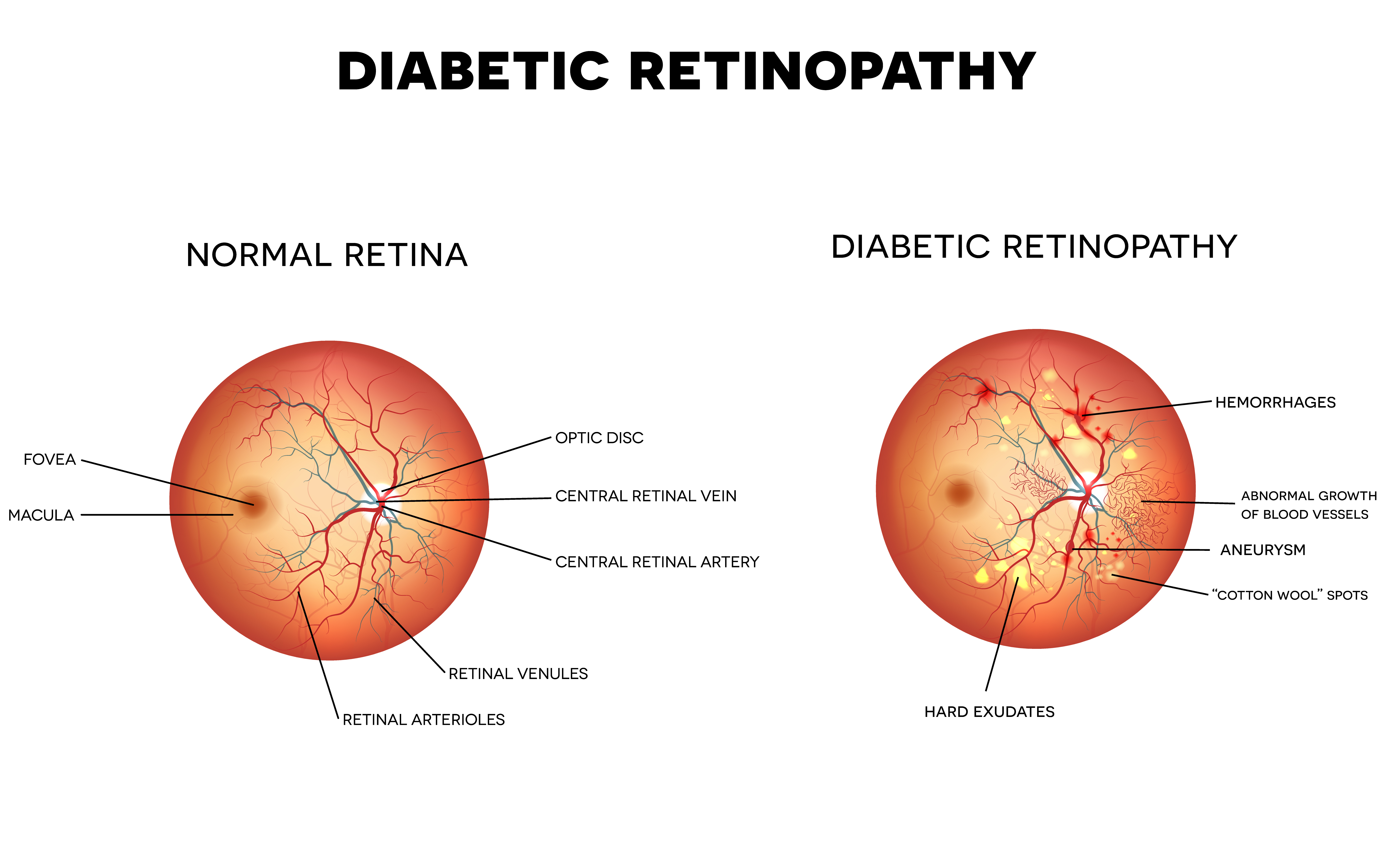
🧠 Pathophysiology (why VEGF rises)
- Chronic hyperglycaemia → pericyte loss, basement-membrane thickening, capillary dropout → retinal ischaemia.
- Ischaemia ↑VEGF → ↑permeability (macular oedema) and fragile neovascularisation (proliferative disease).
🩺 Screening (UK focus)
- Annual mydriatic digital photography (NHS DES). Symptomless until late stages—screening is crucial.
- Pregnancy (pre-existing diabetes): retinal assessment at booking (1st trimester) and again at 28 weeks; if retinopathy at booking, add a review at 16–20 weeks.
🔎 Classification → what it means
- Background (R1): microaneurysms, dot/blot haemorrhages, hard exudates. Usually asymptomatic.
- Pre-proliferative (R2): venous beading, multiple blot haemorrhages, IRMA/cotton-wool spots = significant ischaemia.
- Proliferative (R3): new vessels at disc/elsewhere ± pre-retinal/vitreous haemorrhage → high risk of tractional detachment.
- Maculopathy (M1): macular oedema/exudates within 1 disc diameter of fovea or reduced acuity from oedema.
🚦Referral urgency (practical)
- 🔴 R3 or M1 with reduced vision: urgent same-week ophthalmology (often same-day if vitreous haemorrhage/sudden floaters or vision drop).
- 🟠 R2: prompt routine referral (weeks).
- 🟢 R1: continue annual screening; optimise risk factors.
🧰 Management
- Risk factor optimisation: individualised HbA1c target, strict BP control, statin/ACEi as indicated, smoking cessation.
- Macular oedema (centre-involving): intravitreal anti-VEGF (e.g., aflibercept/ranibizumab); steroids in selected cases.
- Proliferative retinopathy: pan-retinal photocoagulation (PRP); anti-VEGF as adjunct/bridge.
- Advanced disease: vitrectomy for non-clearing vitreous haemorrhage or tractional retinal detachment.
⚠️ Red flags (act now)
- Sudden floaters, curtain over vision, or acute vision drop → possible vitreous haemorrhage/retinal detachment → same-day eye assessment.
- Pregnancy with progressive retinopathy → expedite ophthalmology review.
📚 Teaching diagram placeholders
🧑⚕️ Case vignette
A 58-year-old with T2D (12 yrs), HbA1c 74 mmol/mol, BP 154/92, reports mild central blur. Screening photo shows hard exudates within 1DD of the fovea and thickening on OCT. ✅ M1 maculopathy → refer urgently for anti-VEGF; tighten BP and glucose; start/optimise statin and ACEi.
💡 Mentor tip
If you remember just three things for viva: duration drives risk, VEGF links ischaemia to oedema/neovascularisation, and R3/M1 need urgent eyes-on. Everything else is risk-factor medicine.