Related Subjects:
|Alpha Thalassaemia
|Beta Thalassaemia
|Anaemia of Chronic Disease
|Aplastic anaemia(AML)
|Autoimmune Haemolytic anaemia (AIHA)
Beta Thalassemia Trait is a common hemoglobinopathy characterized by hypochromic microcytic anaemia, the presence of target cells on blood smears, and an increased level of HbA₂ on hemoglobin electrophoresis.
About
- Genetic Basis: Beta Thalassemia Trait is an inherited disorder caused by mutations in one of the two β-globin genes (HBB) located on chromosome 11. It follows an autosomal dominant inheritance pattern.
- Hemoglobin Composition: In adults, hemoglobin (Hb) is composed of two α (alpha) chains and two β (beta) chains (α₂β₂). Beta Thalassemia results from reduced or absent production of β-globin chains.
- Fetal Hemoglobin (HbF): Fetal hemoglobin lacks β-globin chains (γ₂β₂) and remains unaffected until β-globin production decreases postnatally, often unmasking the thalassemia trait.
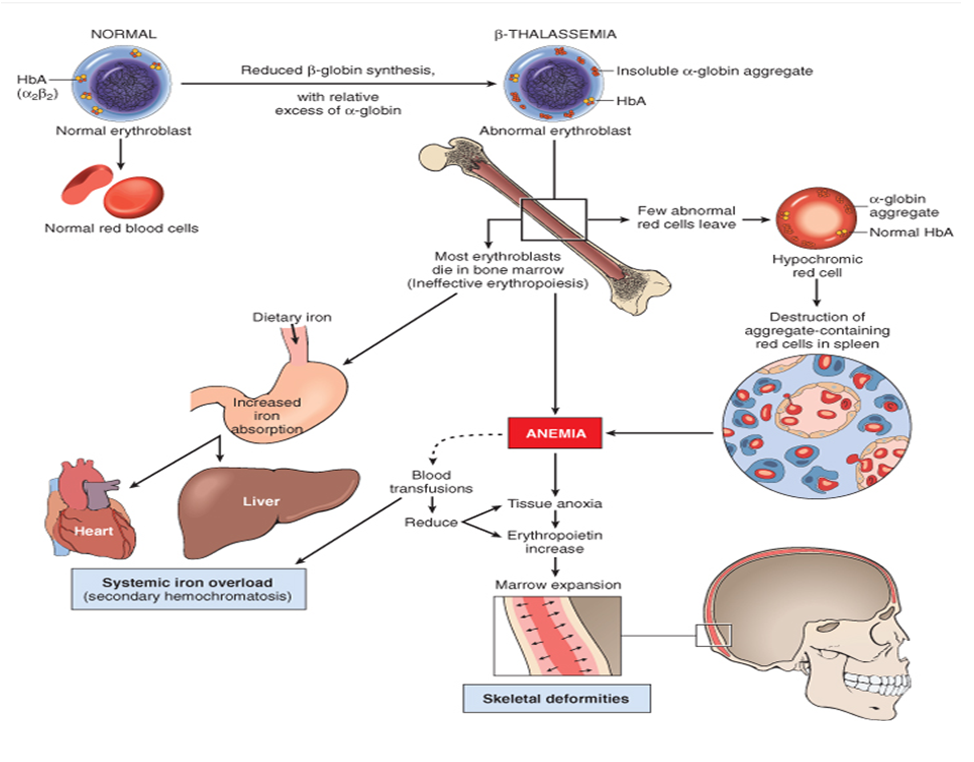
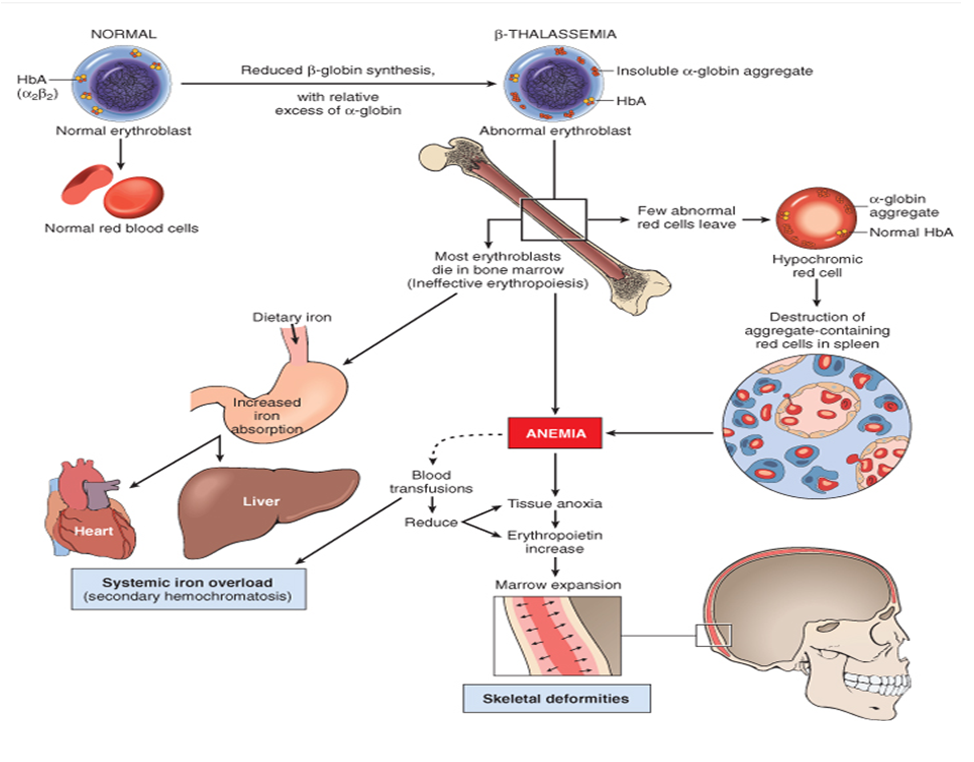
- Pathophysiological Mechanism: The deficiency in β-globin chains leads to an excess of α-globin chains, which form unstable aggregates. These aggregates cause ineffective erythropoiesis and hemolysis, resulting in anaemia.
- Globin Chain Imbalance: The imbalance between α and β chains disrupts the normal hemoglobin synthesis, contributing to the characteristic microcytic and hypochromic red blood cells.
Epidemiology
- Prevalence: Beta Thalassemia Trait is most prevalent in individuals of Mediterranean (e.g., Italian, Greek), Middle Eastern, South Asian (e.g., Indian, Pakistani), and Southeast Asian (e.g., Filipino) descent.
- Carrier Frequency: Carrier rates can range from 1-15% in high-prevalence regions.
- Global Distribution: Due to historical selective advantage against malaria, Beta Thalassemia Trait is common in malaria-endemic areas.
Aetiology
- Genetic Mutations: Over 200 different mutations in the HBB gene have been identified, leading to variable reductions in β-globin chain production.
- Inheritance Pattern: Autosomal dominant; inheriting one mutated gene results in Beta Thalassemia Trait, while inheriting two leads to Beta Thalassemia Major.
- Genetic Counseling: Important for affected families to understand the risk of having children with more severe forms of thalassemia.
Pathophysiology
- Imbalanced Globin Chain Production: Deficiency in β-globin chains leads to excess α-globin chains, which precipitate in red blood cell precursors, causing ineffective erythropoiesis and hemolysis.
- Bone Marrow Expansion: The body compensates for anaemia by expanding erythropoiesis in the bone marrow, leading to bone deformities and marrow hyperplasia.
- Iron Metabolism: While Beta Thalassemia Trait typically does not involve iron overload, individuals may accumulate excess iron if they receive frequent blood transfusions.
- Oxidative Stress: Excess α-globin chains generate reactive oxygen species, contributing to cellular damage and hemolysis.
Classification
- Thalassemia Major (Cooley's Anemia):
- Genetics: Homozygous or compound heterozygous mutations in the HBB gene.
- Clinical Presentation: Severe anaemia, growth retardation, skeletal deformities, and requires regular blood transfusions.
- Complications: Iron overload, heart disease, liver dysfunction, endocrine abnormalities.
- Thalassemia Intermedia:
- Genetics: Less severe mutations compared to Thalassemia Major, often compound heterozygous.
- Clinical Presentation: Moderate anaemia, may require occasional blood transfusions.
- Complications: Similar to Thalassemia Major but less severe; includes iron overload and bone deformities.
- Thalassemia Minor (Trait):
- Genetics: Heterozygous mutations in the HBB gene.
- Clinical Presentation: Usually asymptomatic or mild anaemia, often discovered incidentally during routine blood tests.
- Complications: Generally minimal; however, carriers may experience mild anaemia during physiological stress such as pregnancy.
Clinical Features
- Bone Marrow Expansion:
- Extramedullary Haemopoiesis: Leads to hepatosplenomegaly (enlarged liver and spleen).
- Skull Marrow Expansion: Causes "hair-on-end" appearance on skull X-rays due to bone deformities and osteopenia.
- Iron Overload:
- Results from frequent blood transfusions required in Thalassemia Major and Intermedia.
- Leads to organ damage, including:
- Endocrine Disorders: Hypogonadism, hypothyroidism, diabetes mellitus.
- Cardiac Complications: Cardiomyopathy, arrhythmias.
- Liver Dysfunction: Hepatic fibrosis, cirrhosis.
- Management involves regular iron chelation therapy to prevent organ damage.
- Complications Specific to Thalassemia Trait:
- Generally asymptomatic but may experience:
- Mild anaemia and microcytosis.
- Increased susceptibility to oxidative stress during haemopoietic stress (e.g., pregnancy, infections).
- Potential for mild splenomegaly.
Investigations
- Complete Blood Count (CBC):
- Microcytic Hypochromic Anaemia: Low Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin (MCH).
- Target Cells: Presence of target cells on peripheral blood smear.
- Reticulocyte Count:
- Often elevated due to increased erythropoietic activity.
- Hemoglobin Electrophoresis:
- Increased HbA₂ (α₂δ₂) levels, typically greater than 3.5%.
- Possible increase in HbF (fetal hemoglobin).
- Normal or reduced HbA levels.
- Iron Studies:
- Serum Ferritin: May be normal or elevated, especially in transfusion-dependent patients.
- Serum Iron and Total Iron-Binding Capacity (TIBC): Usually normal or elevated.
- Genetic Testing:
- Identifies specific mutations in the HBB gene, useful for family screening and genetic counseling.
Management
- General Principles:
- Focus on managing anaemia, preventing complications, and maintaining quality of life.
- Specific Treatments:
- Blood Transfusions:
- Used primarily in Thalassemia Major to maintain hemoglobin levels between 9-10 g/dL.
- Frequent transfusions can lead to iron overload, necessitating chelation therapy.
- Iron Chelation Therapy:
- Desferrioxamine: Administered subcutaneously or intravenously to remove excess iron.
- Oral Chelators: Such as Deferasirox and Deferoxamine alternatives for better patient compliance.
- Splenectomy:
- Considered in cases of hypersplenism to reduce transfusion requirements and manage splenomegaly.
- Reduces hemolysis but increases the risk of infections; thus, vaccination and prophylactic antibiotics may be necessary.
- Folate Supplementation:
- Oral folate is essential to support increased erythropoiesis.
- Vitamin C Supplementation:
- High-dose vitamin C can enhance iron excretion but should be used cautiously to prevent hemolysis.
- Hematopoietic Stem Cell Transplantation (HSCT):
- Curative option for severe Thalassemia Major, especially in younger patients with matched donors.
- Associated with significant risks and requires careful patient selection.
- Management of Complications:
- Endocrine Disorders: Regular screening and management of diabetes, hypothyroidism, and hypogonadism.
- Cardiac Care: Monitoring for cardiomyopathy and managing heart failure or arrhythmias as needed.
- Liver Health: Surveillance for hepatic fibrosis or cirrhosis through imaging and liver function tests.
- Bone Health: Addressing osteopenia and osteoporosis with calcium and vitamin D supplementation, and bisphosphonates if necessary.
- Infection Prevention: Prophylactic vaccinations and antibiotics post-splenectomy.
Prognosis
- Thalassemia Major: Without regular blood transfusions and chelation therapy, patients typically do not survive past early childhood. With appropriate management, individuals can live into adulthood, though quality of life may be affected by complications.
- Thalassemia Intermedia: Patients have a better prognosis than those with Thalassemia Major but may still face significant health challenges, including iron overload and organ dysfunction.
- Thalassemia Minor (Trait): Generally excellent prognosis with minimal or no clinical symptoms. Carriers typically lead normal lives without the need for medical intervention.
Prevention and Screening
- Carrier Screening: Essential in high-prevalence populations to identify carriers and provide genetic counseling.
- Genetic Counseling: Offered to carriers and their families to assess the risk of having affected offspring.
- Newborn Screening: Early detection through hemoglobin electrophoresis allows for prompt management and intervention.
- Public Health Initiatives: Education and awareness programs in endemic regions to reduce the incidence of severe thalassemia.
Patient Education and Support
- Education on Disease Understanding: Informing patients about the genetic nature, inheritance patterns, and implications of Beta Thalassemia Trait.
- Lifestyle Modifications: Encouraging a balanced diet rich in folate, managing iron intake, and avoiding unnecessary iron supplements unless prescribed.
- Regular Monitoring: Emphasizing the importance of routine blood tests and screenings to monitor hemoglobin levels and detect complications early.
- Support Groups: Providing access to support networks for emotional and psychological support.
- Emergency Planning: Educating patients on recognizing symptoms of severe anaemia or iron overload and seeking prompt medical attention.
References
- Thalassemia International Federation. (2023). Thalassemia Facts and Statistics.
- World Health Organization (WHO). (2022). Haemoglobinopathies: A public health problem of global dimensions.
- Nicholas, R., & Husain, S. (2019). Beta Thalassemia Trait: Diagnosis and Management. Journal of Clinical Hematology, 8(2), 123-130.
Cases — Beta Thalassaemia
- Case 1 — Child with Severe Anaemia:
A 2-year-old boy of Mediterranean origin presents with irritability, pallor, and abdominal distension. Examination shows hepatosplenomegaly and frontal bossing. Hb is 6.0 g/dL, MCV 62 fL, target cells on blood film. Hb electrophoresis reveals absent HbA, elevated HbF. Diagnosis: Beta Thalassaemia Major.
- Case 2 — Young Adult with Mild Anaemia:
A 20-year-old South Asian woman is incidentally found to have microcytosis on pre-conception blood tests. Hb is 11.2 g/dL, MCV 68 fL, with normal iron studies. Hb electrophoresis shows HbA₂ of 5.5%. She is asymptomatic. Diagnosis: Beta Thalassaemia Trait (Carrier).
- Case 3 — Teenager with Transfusion Complications:
A 15-year-old boy with transfusion-dependent thalassaemia major presents with fatigue and joint pain. He has had regular blood transfusions since infancy. Ferritin is 4200 µg/L, MRI shows hepatic iron overload. Diagnosis: Secondary haemochromatosis from chronic transfusions in Beta Thalassaemia Major.
Teaching Commentary 🩸
Beta thalassaemia results from mutations in the beta-globin gene leading to reduced or absent beta chain synthesis. Severity depends on whether one (trait), two (intermedia) or both genes (major) are affected. The key pathophysiology is ineffective erythropoiesis and chronic haemolysis, with compensatory bone marrow expansion causing skeletal deformities. Diagnosis is by Hb electrophoresis, not iron studies. Management ranges from reassurance in carriers, to lifelong transfusions plus iron chelation in major. Genetic counselling is essential, particularly in high-prevalence populations.