Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Atrial septal defect (ASD)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Congenital Acyanotic Heart Disease |Congenital Cyanotic Heart Disease |Cardiac Embryology |Cyanosis - Central and Peripheral |Down's syndrome (Trisomy 21) |Tetralogy of Fallot |Patent Foramen Ovale (PFO) |Ventricular Septal defect (VSD) |Atrial Septal defect (ASD) |Ebstein anomaly |Eisenmenger's syndrome
🫀 In ASD, the murmur is not due to flow across the septum itself, but rather increased right-sided flow → producing an ejection systolic murmur (ESM) over the pulmonary valve. 🔊 Fixed splitting of S2 is a hallmark. 🧪 Surgery/device closure is usually indicated if Qp:Qs > 1.5 or if there is significant right heart dilatation. 💉 Risk of endocarditis is low.
📖 About
- ASD = congenital defect with an abnormal opening between the atria → left-to-right shunt.
- Results in volume overload of the RA & RV, and ↑ pulmonary blood flow.
- ~10% of congenital heart disease. More common in ♀ and in Down’s syndrome.
⚙️ Pathophysiology
- Oxygenated blood from LA → RA → RV → pulmonary artery → pulmonary hypertension risk.
- RA & RV become dilated over time → right heart failure.
- Chronic shunt may cause pulmonary vascular remodelling → Eisenmenger syndrome (shunt reversal & cyanosis).
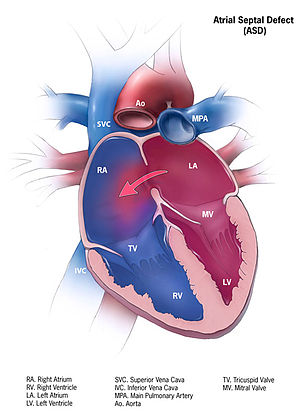
🔎 Types of ASD
- Ostium Secundum (70%): Commonest. Foramen ovale region. Often + mitral valve prolapse. ECG: RBBB + RAD.
- Ostium Primum (15%): Near AV valves → partial AVSD. Often with MR/TR. Associated with Down’s, Noonan, Klinefelter. ECG: RBBB + LAD + 1° AV block.
- Sinus Venosus (15%): Near SVC/IVC. Often anomalous pulmonary venous drainage. ECG: RBBB.
- Unroofed Coronary Sinus (<1%): Rare, coronary sinus drains to LA.
🩺 Clinical Presentation
- Often silent in childhood → may present later.
- Symptoms: Dyspnoea, fatigue, recurrent chest infections, palpitations (AF/flutter).
- Exam:
- 🌟 Fixed, wide split S2.
- ESM at left upper sternal edge (↑ flow across PV).
- Mid-diastolic murmur at LLSE (↑ flow across TV).
- Advanced: Signs of RHF (JVP ↑, hepatomegaly, oedema).
🧪 Investigations
- CXR: Cardiomegaly, pulmonary plethora, enlarged RA/RV.
- ECG:
- Secundum: RBBB + RAD.
- Primum: RBBB + LAD + 1° AV block.
- Echocardiography: Key test – visualises defect, shunt, RV dilatation, valve involvement.
- Cardiac MRI: Detailed anatomy, esp. sinus venosus.
- Right Heart Cath: Measures Qp:Qs ratio & pulmonary pressures.
⚠️ Complications
- 💨 Pulmonary hypertension.
- 📉 Right heart failure.
- ❤️ Atrial arrhythmias (AF/flutter).
- 🧠 Paradoxical embolism → stroke.
- 🔄 Eisenmenger syndrome if untreated.
💊 Management
- Monitoring: Small, asymptomatic ASDs → echo follow-up.
- Closure Indications: Qp:Qs > 1.5 or evidence of RV dilatation.
- Catheter device closure: Secundum defects (minimally invasive).
- Surgical closure: Needed for primum, sinus venosus, or very large secundum ASDs. Operative mortality <1% in specialist centres.
- Anticoagulation: If AF or paradoxical embolism.
- Prognosis: Excellent if repaired before pulmonary HTN develops.
📚 Reference
🩺 Case 1 — Child with Recurrent Chest Infections
A 6-year-old girl is evaluated for recurrent chest infections and poor growth. Exam reveals a fixed split of the second heart sound and a systolic murmur at the left upper sternal edge. Echocardiography shows a secundum ASD with right atrial and right ventricular dilatation. Management: 🩺 Elective closure (percutaneous device or surgical repair) usually in early childhood to prevent long-term complications. Avoid: ❌ Delaying closure beyond adolescence, as this increases risk of pulmonary hypertension and arrhythmias.
🩺 Case 2 — Adult with Incidental Murmur
A 35-year-old woman is found to have a systolic murmur during a routine check. She is asymptomatic, but echo demonstrates a secundum ASD with significant left-to-right shunt (Qp:Qs > 1.5). Management: 💊 Closure indicated if shunt is significant and RV dilatation present, even if asymptomatic. Endocarditis prophylaxis not routinely required. Avoid: ❌ Assuming asymptomatic means benign — late complications (AF, RV failure) can still occur.
🩺 Case 3 — Elderly Patient with Pulmonary Hypertension
A 70-year-old man presents with exertional dyspnoea and ankle swelling. Exam shows elevated JVP, a loud P2, and a systolic murmur. Echo confirms an unrepaired secundum ASD with severe pulmonary hypertension and right heart failure. Management: 🚑 Supportive therapy for right heart failure (diuretics, oxygen). ASD closure not advised if pulmonary vascular resistance is very high and right-to-left shunt has developed (Eisenmenger physiology). Palliative and specialist pulmonary hypertension care considered. Avoid: ❌ Closing the defect in irreversible pulmonary hypertension — can worsen right-sided failure.