Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Parkinson disease
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:Multiple System Atrophy (MSA) |Parkinson Plus syndromes |Parkinsonism |Idiopathic Parkinson disease |Progressive Supranuclear Palsy |Drug Induced Parkinson disease |Neuroleptic Malignant Syndrome
🧠 Parkinson's Disease (PD) is a chronic, progressive neurological disorder affecting movement and non-motor functions. 👴 Most often seen in older adults, though genetic forms can present earlier.
About
- 🌀 Idiopathic PD: Tremor, rigidity, bradykinesia.
- 👵 More common in elderly, but younger onset with genetic variants.
Aetiology
- ⬇️ Dopaminergic neurons lost in the substantia nigra.
- ⚡ Disrupted communication in the basal ganglia.
- 🧩 Lewy bodies (α-synuclein inclusions) hallmark of PD pathology.
Pathology: Braak Staging
- 📈 Pathology spreads stepwise: brainstem → midbrain → cortex.
- 🚽 Early = constipation, REM sleep disorder; 🤲 Later = tremor, rigidity.
Genetics
- 🧬 PARK1 (α-synuclein): Early-onset, autosomal dominant.
- 🧬 PARK2 (parkin): Autosomal recessive, good response to L-Dopa.
Clinical Features
- ✋ Tremor: “Pill-rolling” resting tremor.
- 🐢 Bradykinesia: Slowness, difficulty initiating movement.
- 🪵 Rigidity: Limb stiffness, cogwheeling.
- ⚖️ Postural instability: Falls, poor balance.
- 🌙 Non-motor: depression, constipation, sleep disturbance, anosmia.
Stages of PD
- 1️⃣ Mild unilateral tremor.
- 2️⃣ Bilateral symptoms, slower movement.
- 3️⃣ Falls, significant motor difficulty.
- 4️⃣ Severe disability, daily assistance required.
- 5️⃣ Bedridden/wheelchair, hallucinations possible.
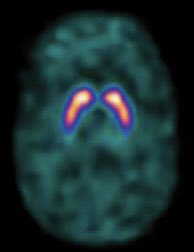
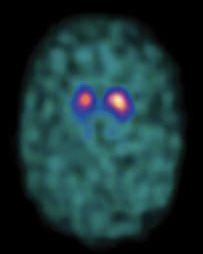
Diagnostic Imaging
- 🧲 MRI: Exclude mimics (vascular PD, NPH).
- 📊 DaT Scan: Differentiates PD from essential tremor.
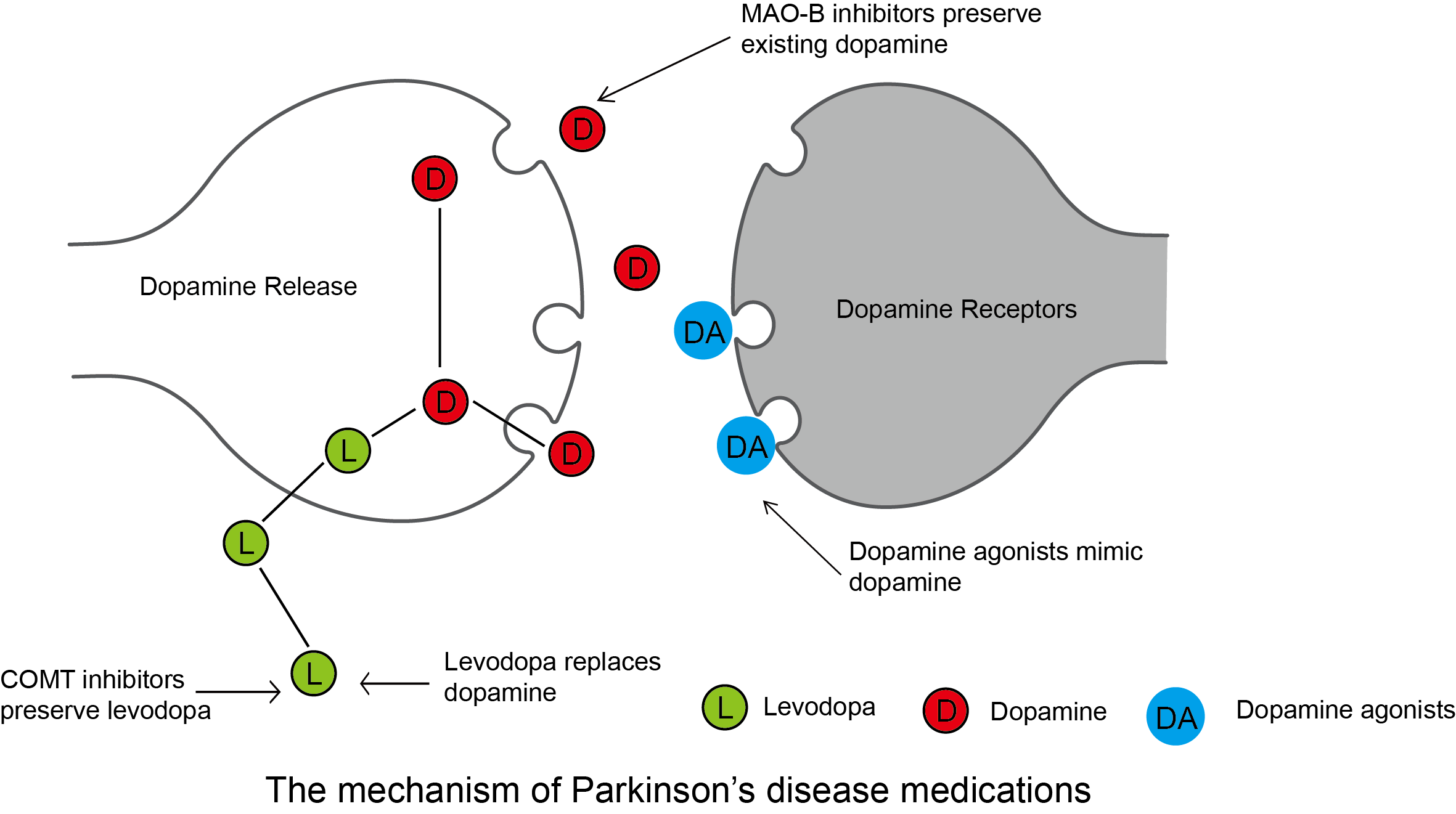
Pharmacological Management
- 💊 Levodopa + Carbidopa (Sinemet): Gold standard, best for motor symptoms.
- 🟤 COMT inhibitors: Prolong levodopa action (e.g. entacapone).
- 🟢 Dopamine agonists: Ropinirole, pramipexole (younger patients).
- 🔵 MAO-B inhibitors: Rasagiline, selegiline (mild disease).
- 🟣 Anticholinergics: Tremor-dominant PD (younger patients).
- 🟡 Amantadine: Useful for dyskinesias.
🧠 About Parkinson’s Drug Management
- Parkinson’s disease is due to dopamine deficiency in the basal ganglia.
- Main goal: restore dopaminergic activity, reduce motor symptoms, and improve quality of life.
- Treatment is individualised based on age, frailty, cognition, and comorbidities.
💊 Main Drug Classes & Dosing
- 1️⃣ Levodopa + DDC inhibitor (co-careldopa, co-beneldopa)
- First-line in patients >70 or with cognitive impairment.
- Dose:
- Start low (e.g. co-careldopa 12.5/50 mg TDS) and titrate.
- Usual range: 50/200 mg TDS–QDS. Adjust according to response.
- ⚠️ Side effects: dyskinesias, motor fluctuations (on–off), hallucinations, hypotension.
- 2️⃣ Dopamine Agonists (pramipexole, ropinirole, rotigotine patch, apomorphine)
- Pramipexole: start 0.125 mg TDS → titrate to max 1.5 mg TDS.
- Ropinirole: start 0.25 mg TDS → titrate; XL forms available.
- Rotigotine patch: start 2 mg/24 h → titrate to max 16 mg/24 h.
- Apomorphine (SC): rescue injections or continuous infusion under specialist supervision.
- ⚠️ Side effects: impulse control disorders, hallucinations, oedema, somnolence.
- 3️⃣ MAO-B Inhibitors (selegiline, rasagiline, safinamide)
- Selegiline: 5 mg OD or BD.
- Rasagiline: 1 mg OD.
- Safinamide: 50 mg OD → may increase to 100 mg OD.
- ⚠️ Side effects: insomnia, hallucinations, hypertensive crisis with tyramine foods (rare).
- 4️⃣ COMT Inhibitors (entacapone, opicapone, tolcapone)
- Entacapone: 200 mg with each levodopa dose (max 10/day).
- Opicapone: 50 mg OD at bedtime.
- Tolcapone: 100–200 mg TDS (⚠️ hepatotoxicity risk).
- ⚠️ Side effects: diarrhoea, urine discolouration, hepatotoxicity (tolcapone).
- 5️⃣ Amantadine
- Dose: 100 mg OD–BD (max 300 mg/day).
- Useful for levodopa-induced dyskinesias.
- ⚠️ Side effects: livedo reticularis, ankle oedema, confusion.
- 6️⃣ Anticholinergics (trihexyphenidyl, procyclidine)
- Dose: Trihexyphenidyl 1 mg OD–BD (max 15 mg/day).
- More effective for tremor-predominant PD in young patients.
- ⚠️ Side effects: confusion, urinary retention, dry mouth → avoid in elderly.
📋 NICE Simplified Pathway
- 👴 Older (>70) or cognitive impairment → Levodopa.
- 🧑 Younger (<70), no cognitive issues → Dopamine agonist or MAO-B inhibitor.
- ⚡ Escalate stepwise with COMT inhibitors, dopamine agonists, or amantadine if fluctuations develop.
- Specialist referral at all treatment stages.
🚑 Management When Unable to Swallow (NBM)
- 💧 Dispersible levodopa (Madopar® dispersible): can be given via NG tube.
- 🩹 Rotigotine patch: provides continuous dopaminergic stimulation.
- 💉 Apomorphine (SC injection/infusion): specialist initiation, useful for acute rescue.
- 📡 Duodopa® (levodopa–carbidopa intestinal gel): continuous PEG-J infusion.
- ⚠️ Never stop dopaminergic drugs suddenly → risk of Parkinsonism–Hyperpyrexia Syndrome.
⚠️ Key Cautions & Monitoring
- Impulse control disorders (gambling, hypersexuality, binge eating) with dopamine agonists.
- Hallucinations & psychosis with dopaminergic drugs.
- Postural hypotension with levodopa and dopamine agonists.
- Monitor LFTs with tolcapone.
- Adjust doses in renal impairment for amantadine.
Surgical
- 🧩 Deep Brain Stimulation (DBS): For advanced disease, subthalamic nucleus/globus pallidus targets.
Multidisciplinary Care
- 👩⚕️ Nurse specialist: medication timing, education.
- 🏃 Physiotherapy: balance, gait training.
- 🗣️ SLT: dysarthria, dysphagia.
- 🛠️ OT: adaptive aids, safety at home.
Hospital/Acute Considerations
- ⏰ Never delay PD meds (risk of severe deterioration, even NBM use NG or rotigotine patch).
- 🚫 Avoid antidopaminergic drugs (metoclopramide, haloperidol, prochlorperazine).
Non-Motor Complications
- 🚽 Constipation → macrogol, fluids, mobility.
- 📉 Orthostatic hypotension → fludrocortisone, midodrine.
- 🦠 Recurrent UTIs → hydration, constipation prevention.
- 👻 Psychosis/hallucinations → quetiapine, clozapine.
- 🧩 Dementia → rivastigmine (watch for tremor worsening).
Advance Care Planning
- 📝 Advance directives, lasting power of attorney.
- 🤝 Signposting to community support and respite care.
References
Cases — Parkinson’s Disease with Complications
- Case 1 — Motor Fluctuations (“Wearing Off”) ⏳: A 68-year-old man on levodopa for 7 years reports that tremor and rigidity return 3 hours after each dose. He experiences “on–off” fluctuations through the day. Complication: Motor fluctuations due to long-term levodopa use. Management: Shorten levodopa dosing intervals; add COMT inhibitor (entacapone) or dopamine agonist.
- Case 2 — Dyskinesias 💃: A 62-year-old woman develops involuntary writhing movements of her trunk and arms about 30 minutes after each levodopa dose. Complication: Levodopa-induced dyskinesia. Management: Lower levodopa dose; add amantadine; consider deep brain stimulation if severe.
- Case 3 — Parkinson’s Disease Dementia 🧠: A 75-year-old man with 10 years of PD develops progressive memory loss, visual hallucinations, and difficulty with daily tasks. Complication: Parkinson’s disease dementia. Management: Rivastigmine (first-line cholinesterase inhibitor); review dopaminergic drugs that worsen hallucinations.
- Case 4 — Autonomic Dysfunction 💧: A 70-year-old woman with PD reports frequent faints on standing, constipation, and urinary urgency. BP falls from 135/80 supine to 95/60 standing. Complication: Autonomic dysfunction (orthostatic hypotension, bladder involvement). Management: Non-pharmacological (slow position changes, compression stockings, ↑ salt/fluid); consider fludrocortisone or midodrine.
- Case 5 — Impulse Control Disorder 🎰: A 60-year-old man on pramipexole for PD develops compulsive gambling and hypersexuality, which his wife finds distressing. Complication: Dopamine agonist–induced impulse control disorder. Management: Reduce/stop dopamine agonist; switch to levodopa-based regimen; behavioural support.
Teaching Commentary 🧠
Parkinson’s disease complications can be divided into: - Motor: fluctuations (“wearing off”), dyskinesias. - Neuropsychiatric: dementia, hallucinations, depression, impulse control disorders. - Autonomic: postural hypotension, constipation, bladder dysfunction, erectile dysfunction. - Sleep: REM sleep behaviour disorder, insomnia. Complications often reflect both disease progression and treatment side effects. Management requires balancing dopaminergic therapy, adding adjuncts (COMT/MAO-B inhibitors), and addressing non-motor symptoms with MDT support. Deep brain stimulation is an option in selected patients with refractory motor fluctuations.