Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Hypothyroidism
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
💡 Always start with a lower dose of levothyroxine in the elderly and in those with angina or heart failure, to avoid precipitating arrhythmia or ischaemia.
📖 Introduction
- Hypothyroidism = inadequate thyroxine production for normal metabolism.
- Thyroid produces both T4 and T3, but T3 is the active form at tissue level.
- TSH is the best single test: ↑TSH is a highly sensitive marker of primary hypothyroidism.
- A normal TSH in a treated patient usually indicates adequate replacement and euthyroidism.
⚙️ Aetiology
- Primary hypothyroidism (95%): intrinsic thyroid failure (iodine deficiency, autoimmune thyroiditis, post-surgical, post-radioiodine).
- Secondary hypothyroidism: pituitary or hypothalamic disease → insufficient TSH secretion (TSH low/normal despite low T4).
🧬 Causes of Primary Hypothyroidism
- Iodine deficiency: still the most common cause worldwide.
- Autoimmune: Hashimoto’s thyroiditis (± goitre) or atrophic thyroiditis (no goitre). Often associated with other autoimmune disease.
- Post-ablative: surgery, radioiodine, external radiotherapy.
- Drugs: carbimazole, propylthiouracil, lithium, amiodarone, interferons, thalidomide, rifampicin, excess iodine (e.g. kelp supplements).
- Transient thyroiditis: subacute (de Quervain’s), often post-viral, painful goitre.
- Postpartum thyroiditis: transient hyper → hypo → recovery within 1 year.
- Infiltrative disease: amyloidosis, sarcoidosis, haemochromatosis, TB, scleroderma.
- Congenital: agenesis, hypoplasia, ectopic gland, or enzyme defects (causes cretinism if untreated).
🧑⚕️ Clinical Features
- General: tiredness, lethargy, weight gain, cold intolerance.
- Neuropsychiatric: poor memory, depression, psychosis, ataxia, slow movements.
- GI: constipation.
- Reproductive: menorrhagia or oligomenorrhoea, infertility.
- Skin/hair: dry skin, thin brittle hair, hair loss, periorbital puffiness.
- Cardio: bradycardia, heart failure, pericardial effusion.
- Neuro exam: “hung-up” slow-relaxing reflexes, proximal myopathy.
- Severe: myxoedema coma (rare, emergency).
- Children: congenital hypothyroidism → growth retardation & cretinism if untreated.
🆚 Differential Diagnosis
- Hypopituitarism (low/normal TSH with low T4).
- Chronic fatigue syndrome.
- Depression (can mimic fatigue/low mood).
- Obstructive sleep apnoea.
- Other causes of weight gain and lethargy (e.g. Cushing’s, anaemia).
🔬 Investigations
- TFTs: high TSH, low T4 (primary); low/normal TSH with low T4 (secondary).
- FBC: normocytic or macrocytic anaemia (pernicious anaemia association).
- CXR: may show pleural/pericardial effusion.
- ECG: bradycardia, low QRS voltage.
- Thyroid antibodies: TPO antibodies positive in autoimmune thyroiditis.
- Ultrasound: if nodules/goitre present.
📊 Classification
- Overt hypothyroidism: TSH ↑ (>10 mU/L), T4 ↓ → treat.
- Subclinical hypothyroidism: TSH ↑, T4 normal. Treat if TSH >10, symptomatic, or TPO-Ab positive.
- Secondary hypothyroidism: T4 ↓ with inappropriately low/normal TSH → pituitary cause.
- Euthyroid: normal TSH & T4.
📉 ECG in Hypothyroidism
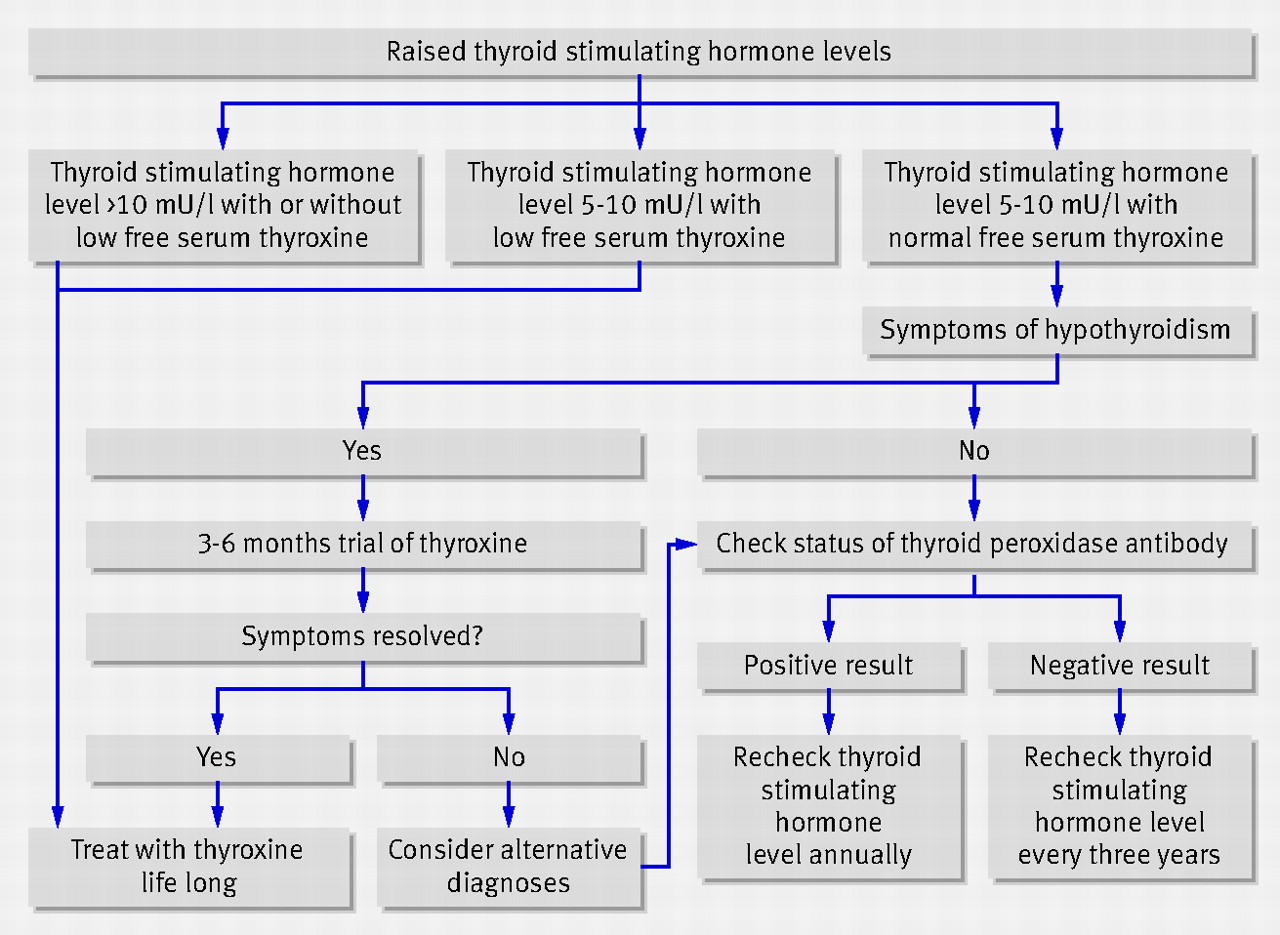
🧪 Treatment Algorithm
💊 Management
- Levothyroxine (T4): first-line, lifelong replacement in most patients.
- Dosing: Typical adult dose 100–150 mcg OD. Start lower (25–50 mcg) in elderly or those with ischaemic heart disease, then titrate every 6–8 weeks.
- T3 (liothyronine): only indicated in selected cases (e.g. myxoedema coma, rare poor responders to T4).
- Monitor: TSH (and T4 in secondary hypothyroidism). Target TSH in normal range.
- Pregnancy: higher levothyroxine requirements; check TFTs early each trimester.
- Myxoedema coma: ICU emergency — IV levothyroxine ± liothyronine, IV hydrocortisone, supportive care.
📌 OSCE / Exam Tips
- Classic vignette: young woman with fatigue, cold intolerance, dry skin, TSH ↑, T4 ↓.
- Differentiate subclinical vs overt hypothyroidism.
- In elderly/IHD → start levothyroxine low & slow.
- Myxoedema coma: hypothermia, bradycardia, drowsiness → emergency.
- Don’t forget associations: autoimmune thyroiditis + pernicious anaemia / T1DM.
📚 References
- Hypothyroidism: An Update – AAFP
- Kumar & Clark’s Clinical Medicine, 10th ed.
- NICE CKS: Hypothyroidism (2023).
🧾 Clinical Case Examples – Hypothyroidism
Case 1 – Classic Overt Hypothyroidism 👩🦰 A 32-year-old woman presents with 6 months of fatigue, weight gain, constipation, and feeling cold all the time. Exam: dry skin, periorbital puffiness, slow reflexes. Bloods: TSH 18 mU/L, T4 low, TPO antibodies positive. 👉 Diagnosis: Autoimmune hypothyroidism (Hashimoto’s). 👉 Management: Start levothyroxine 100 mcg daily, monitor TSH every 6–8 weeks. Lifelong therapy likely.
Case 2 – Elderly with IHD & Hypothyroidism ❤️ A 75-year-old man with ischaemic heart disease presents with lethargy and ankle swelling. Exam: bradycardia (HR 52), pitting oedema, cool peripheries. Bloods: TSH 12 mU/L, T4 low. 👉 Key point: Elderly patient with cardiac disease — risk of precipitating angina/arrhythmia if started on high-dose thyroxine. 👉 Management: Start low-dose levothyroxine (25 mcg OD), titrate slowly, close cardiac monitoring.
Case 3 – Myxoedema Coma 🚨 A 68-year-old woman with known untreated hypothyroidism is brought in drowsy, hypothermic (34°C), and bradycardic (HR 40). Exam: periorbital puffiness, hypotension, delayed reflexes. Bloods: very low T4, very high TSH, hyponatraemia. 👉 Diagnosis: Myxoedema coma — rare, life-threatening hypothyroidism. 👉 Management: ICU admission, IV levothyroxine ± liothyronine, IV hydrocortisone (until adrenal insufficiency excluded), active warming, fluid/electrolyte correction, treat precipitant (e.g. infection, MI).