Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Carbon Monoxide Toxicity
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Drug Toxicity - clinical assessment |Metabolic acidosis |Aspirin or Salicylates toxicity |Ethylene glycol toxicity |Ethanol toxicity |Methanol toxicity |Ricin toxicity |Carbon Tetrachloride Toxicity |Renal Tubular Acidosis |Lactic acidosis |Iron Toxicity |Tricyclic Antidepressant Toxicity |Opiate Toxicity |Carbon monoxide Toxicity |Benzodiazepine Toxicity |Paracetamol (Acetaminophen) toxicity |Amphetamine toxicity |Beta Blocker toxicity |Calcium channel blockers toxicity |Cannabis toxicity |Cyanide toxicity |Digoxin Toxicity |Lithium Toxicity |NSAIDS Toxicity |Ecstasy toxicity |Paraquat toxicity |Quinine toxicity |SSRI Toxicity |Theophylline Toxicity |Organophosphate (OP) Toxicity |Toxin elimination by dialysis |Drug Toxicity with Specific Antidotes
🚨 Carbon Monoxide (CO) Poisoning → Invisible, odourless, colourless gas ⚠️. Not detected by a pulse oximeter ❌ (SpO₂ unreliable). Diagnosis = 🩸 ABG with carboxyhaemoglobin (CoHb). Prognosis depends on ⏱️ rapid removal from source + 100% O₂ therapy. Normal CoHb <10% (up to 10% in smokers 🚬). Severe >30% 🟥.
| 🔥 Moderate/Severe Carbon Monoxide Toxicity |
|---|
|
ℹ️ About
- CO binds Hb with 240× affinity of O₂ → forms CoHb 🩸.
- Shifts O₂–Hb curve left ⬅️ → impaired O₂ release to tissues.
- Also inhibits mitochondrial cytochrome oxidase → blocks electron transport chain → cellular hypoxia ⚡.
- Half-life: 320 min (room air) → 80 min (100% O₂) → 20–30 min (HBOT).
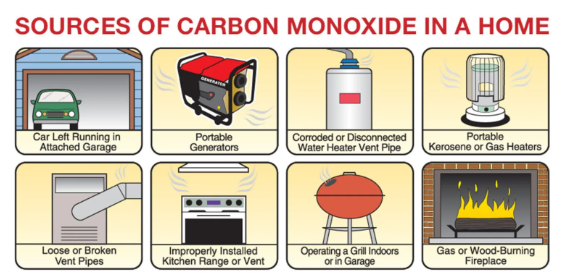
🔎 Aetiology
- 🏠 Faulty boilers, heaters, poorly ventilated gas appliances.
- 🚗 Vehicle exhaust fumes in enclosed space.
- 🔥 House fires (common in winter).
- ⚙️ Occupational exposure: welders, industrial workers.
🩺 Clinical Features
- Early: Headache 🤕, dizziness, nausea, malaise.
- Neuro: Confusion, irritability, seizures, coma 🧠.
- Cardiac: Chest pain, arrhythmias, ischaemia ❤️.
- Skin: "Rosy/pink" appearance 🌹 (misleading sign).
- Delayed sequelae: Memory loss, personality change, parkinsonism (post-hypoxic encephalopathy) 🧠⏳.
🔬 Investigations
- 🩸 ABG: CoHb level (gold standard). Often lactic acidosis from hypoxia.
- FBC: check for polycythaemia in chronic cases.
- U&E, lactate, CK/troponin (myocardial/renal injury).
- ECG: arrhythmias, ischaemia.
- CT head: if coma or persistent neurological symptoms.
📊 Assessing CoHb Levels
- Normal: 1–3% (non-smokers), up to 10% in smokers 🚬.
- >10% = exposure, >20% = symptomatic, >30–40% = severe 🔴.
- Pregnancy: fetal Hb binds CO tighter → increased risk 👶.
💊 Management
- 📞 Call NPIS/TOXBASE for guidance.
- ABC + 100% O₂ at 15 L/min via non-rebreather until CoHb <5%.
- 💉 IV fluids: correct dehydration & support renal function.
- ❤️ ECG & cardiac monitoring for ischaemia/arrhythmias.
- 🧠 Neuro checks for cerebral oedema. Consider mannitol if raised ICP.
- HBOT: if CoHb >25%, neuro/cardiac involvement, pregnancy, or coma.
⚠️ Complications
- 🧠 Delayed neuro sequelae: memory deficits, cognitive decline, parkinsonism.
- ❤️ Cardiac: MI, arrhythmias, heart failure.
- 📉 Multi-organ dysfunction due to persistent hypoxia.
- 👶 Pregnancy: fetal death or developmental issues.
🛡️ Prevention
- 🏠 CO detectors near bedrooms & gas appliances.
- 🔧 Regular servicing of boilers, heaters, chimneys.
- 🌬️ Ensure proper ventilation of fuel-burning appliances.
- 📢 Public education campaigns (esp. winter months).
Case 1 – “Flu” at home that isn’t
A 34-year-old and two family members develop morning headache, nausea, dizziness that improve when outside; boiler recently serviced. Vitals normal; SpO₂ 98% on air (can be falsely reassuring). ABG with co-oximetry shows COHb 18%. Manage with 100% high-flow oxygen via non-rebreather until COHb <5% and symptoms settle; do ECG/troponin and neuro exam. Ventilate the property, switch off the appliance, and advise calling the UK Gas Emergency Service (0800 111 999)/Gas Safe engineer to inspect. Discharge with CO alarm advice and safety-netting for neuro symptoms.
Case 2 – High-risk exposure (pregnancy)
A 28-year-old pregnant woman has syncope and confusion after time in a garage with a running car; exam: mild ataxia. SpO₂ 99% on air; COHb returns at 12% (maternal) but fetus is more vulnerable. Start 100% oxygen immediately, continuous fetal monitoring, labs/ECG. Discuss hyperbaric oxygen with a specialist (consider for pregnancy, neurological signs, loss of consciousness, cardiac