Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Fractured Neck of Femur/Femoral Neck
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Fractured Neck of Femur |Fractured Shaft Femur |Supracondylar Femur Fractures |Femoral fractures and Injuries
⚠️ Key Point: Intracapsular fractures have a higher incidence of AVN (Avascular Necrosis) and non-union due to the femoral head blood supply. 👉 If displacement is minimal → internal fixation gives best outcome. 👉 If displaced → high risk of AVN, so prosthesis insertion is usually required.
ℹ️ About
- 🦴 Intracapsular fractures carry high AVN risk.
- ☠️ 30% of patients die within 1 year.
- 👵 Most common in the elderly due to frailty and falls.
- 🧓 Patients often have multiple co-morbidities.
- 🦴 Osteoporosis is the major underlying factor.
📊 Epidemiology
- ~80,000 hip fractures per year in the UK.
- Numbers are rising as the population ages.
🧠 Anatomy
🧬 Aetiology
- Falls + Osteoporosis are the commonest causes.
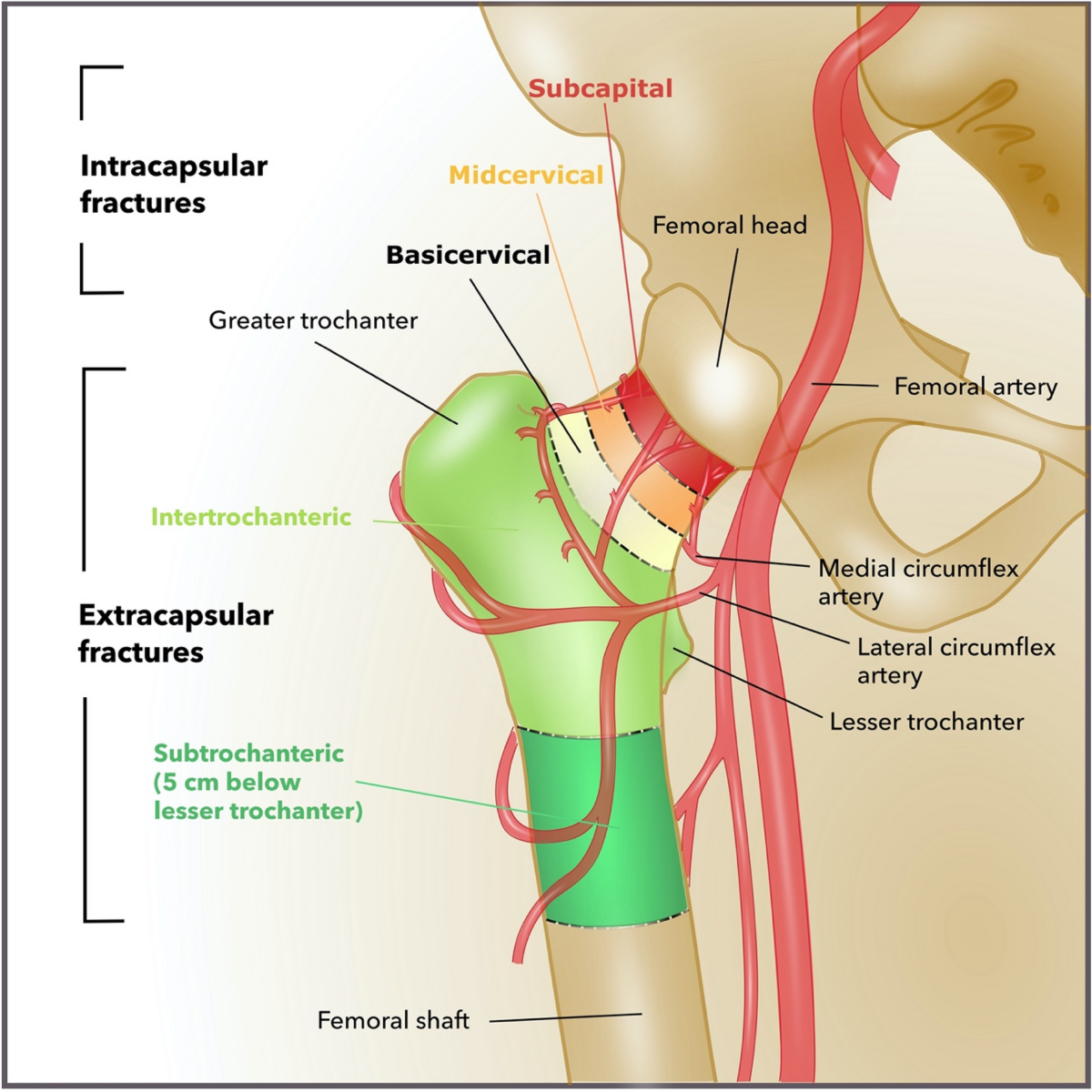
- The medial femoral circumflex artery supplies the femoral head ➝ vulnerable in NOF fractures.
- Vascular compromise ➝ ischaemia ➝ AVN.
📉 Risk Factors for Bone Fragility
- Osteoporosis: age, inactivity, smoking, alcohol, low BMI, family history.
- Previous fragility fracture ➝ doubles future fracture risk.
- Other causes: metastases, Paget’s disease, osteomalacia, hyperparathyroidism, myeloma.
🤕 Risk Factors for Falls
- Muscle weakness, gait or balance problems.
- Neurological diseases: Parkinson’s, stroke.
- Poor vision.
- Medications: sedatives, hypnotics, diuretics, antihypertensives, alcohol.
🩺 Clinical Features
- Pain + external rotation, adduction, and shortening of the affected leg.
- History: establish whether mechanical fall or medical cause (syncope, arrhythmia, hypotension).
- Check co-morbidities that influence management.
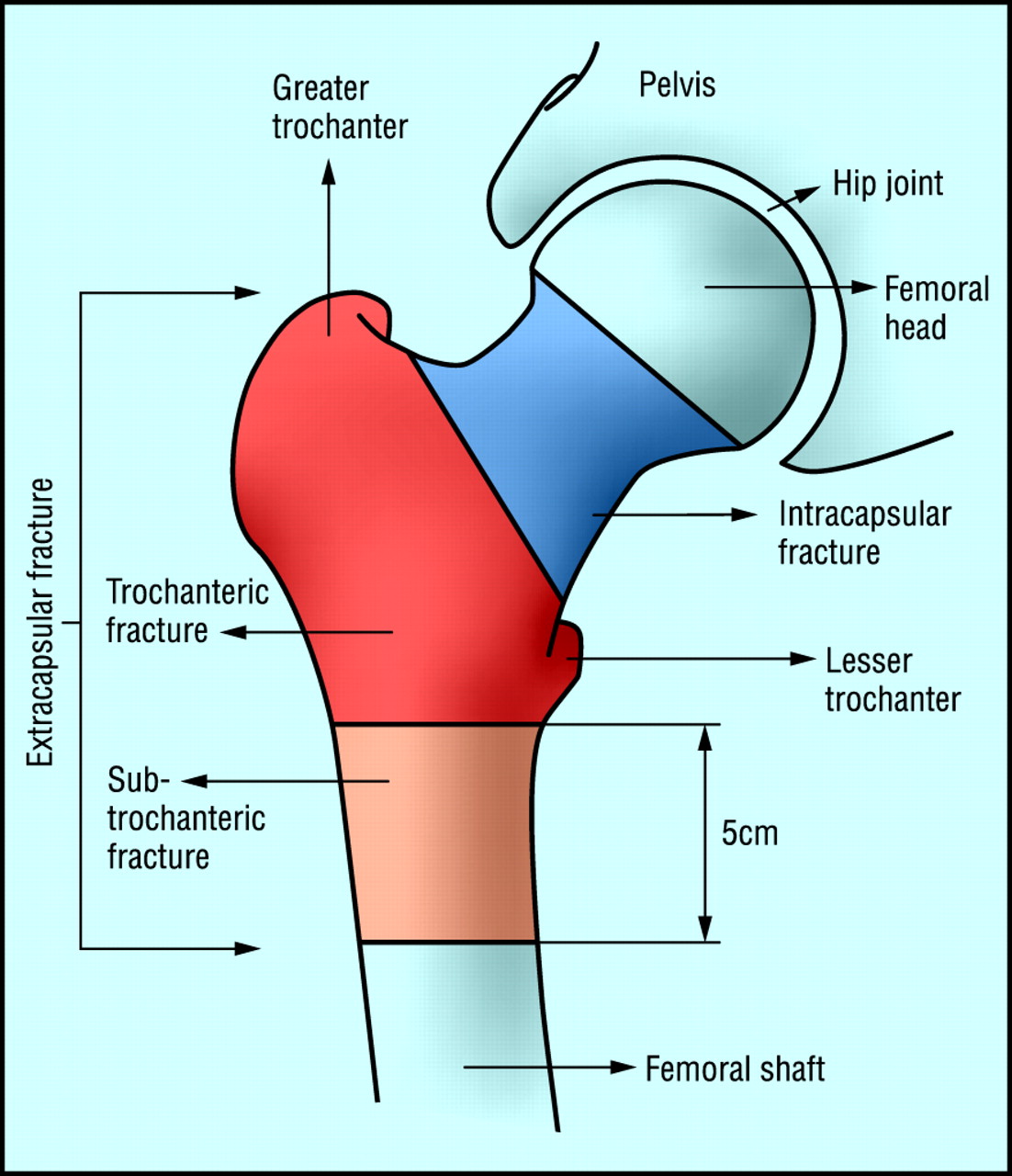
📌 Types of Fracture
- Intracapsular: High risk of AVN + non-union. Tx = hemiarthroplasty/THR.
- Subcapital & Transcervical: Common intracapsular fracture patterns.
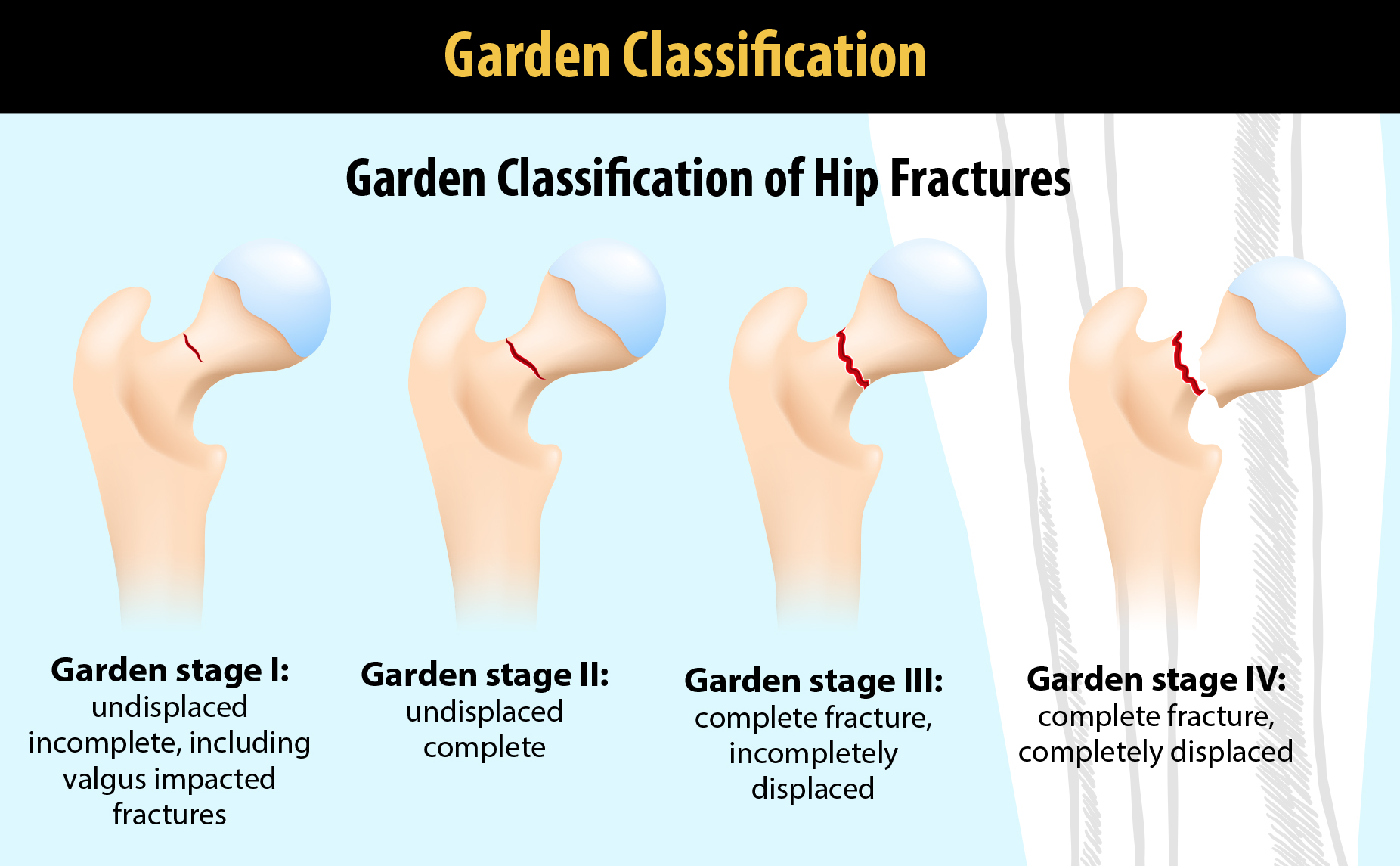
🗂️ Garden Classification
- Type I: Incomplete fracture
- Type II: Complete, undisplaced
- Type III: Complete, partially displaced
- Type IV: Complete, fully displaced
📌 Extracapsular Fractures
- Trochanteric
- Transtrochanteric
- Subtrochanteric
Other Fractures
- Pubic ramus fractures (usually conservative).
- Acetabular fractures (conservative unless complex).
🔍 Investigations
- Baseline bloods: FBC, U&E, clotting, group & save.
- CXR + ECG (pre-op assessment).
- Pelvic AP X-ray (compare both hips, check pubic rami).
- Lateral hip X-ray (often diagnostic when AP is normal).
- MRI/CT if X-rays inconclusive (10% occult fractures).
🛡️ Prevention
- Falls risk assessment + home/environment modifications.
- Muscle strengthening + balance retraining (e.g. Tai Chi).
- Bisphosphonates increase bone density, reduce fracture risk.
- Calcium, Vitamin D, ± HRT can reduce risk.
📊 Mortality: 10% at 30 days, 30% at 12 months (reflecting frailty + co-morbidities).
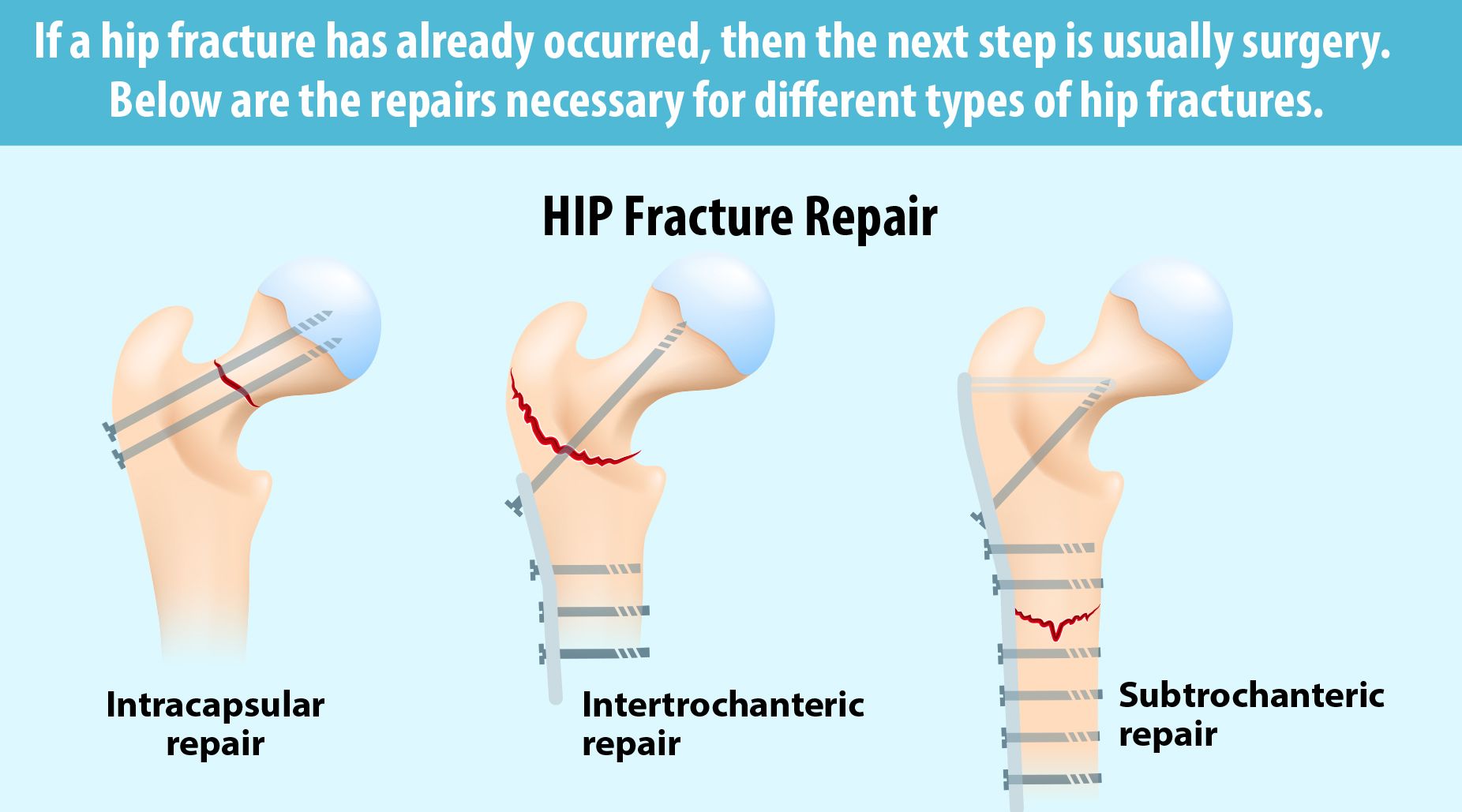
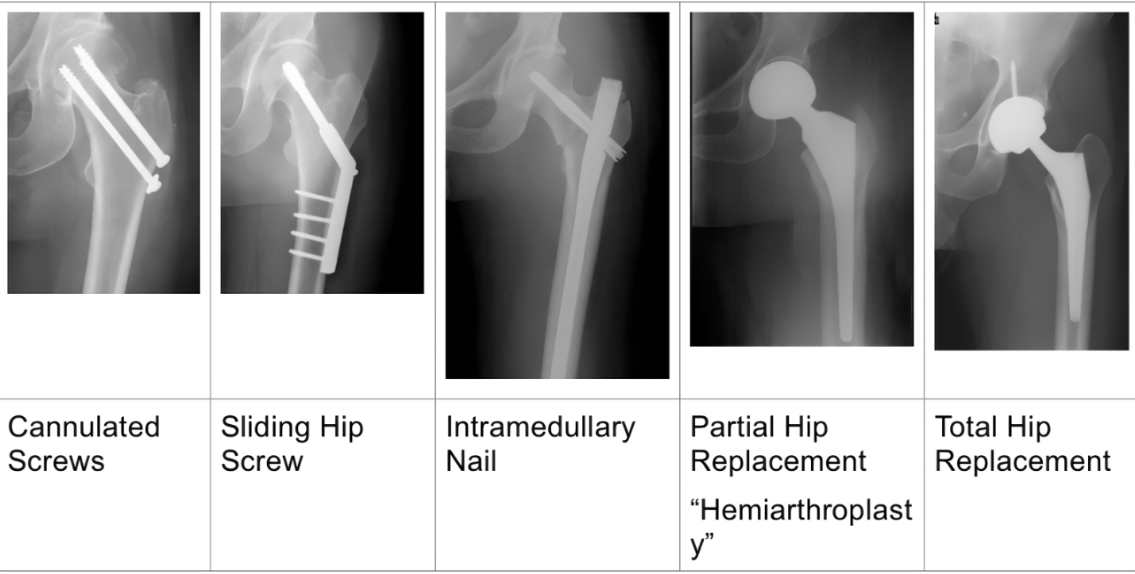
🛠️ Treatment Options
- Conservative: For patients unfit for surgery ➝ bed rest, analgesia, physio. Poor outcomes.
- Surgical: Standard of care.
- Internal fixation: For undisplaced intracapsular (cannulated screws/DHS). Also for young with displaced fractures.
- Hemiarthroplasty: For older patients with displaced fractures ➝ faster recovery.
- Total Hip Replacement (THR): For active elderly/younger displaced fractures ➝ better function long term, higher surgical risk.
- Intramedullary nailing: For extracapsular/subtrochanteric fractures ➝ early mobilisation.
- DHS: For intertrochanteric fractures ➝ controlled collapse and healing.
In frail elderly after a hip fracture, annual IV zoledronate not only prevents further fractures but also reduces mortality. This is unique among osteoporosis treatments and why geriatricians are so keen to give it post-fracture. 5 mg IV once yearly, infused over at least 15 minutes. Ensure adequate vitamin D and calcium before infusion (correct hypocalcaemia).
🩺 Management
- ABC resuscitation.
- Analgesia (including fascia iliaca block).
- IV fluids & electrolyte correction.
- Orthogeriatric review early.
- Admit + imaging if unable to walk or occult fracture suspected.
- Assess mental state, pressure sore risk, nutrition.
- Surgery:
- Intracapsular undisplaced ➝ cannulated screws.
- Intracapsular displaced ➝ hemiarthroplasty or THR if fit.
- Extracapsular ➝ screws/nailing depending on pattern.
- VTE prophylaxis ➝ stockings + LMWH/DOAC until mobilising.
🏃♀️ Post-Surgical Care & Rehabilitation
- Early mobilisation with physio ➝ prevents DVT, improves outcomes.
- Pain management + infection prophylaxis.
- Monitor for complications: infection, non-union, prosthetic dislocation.
- Rehab programmes: strength, balance, gait training ➝ reduce future falls.
⚠️ Complications
- AVN (esp. intracapsular fractures).
- Non-union (esp. displaced fractures).
- Osteoarthritis.
- DVT/PE.
- Surgical site infection, prosthetic dislocation.
📈 Prognosis
- Outcome depends on age, co-morbidities, and rapidity of surgery.
- Mortality: ~30% at 1 year, largely due to frailty not fracture itself.
- Good surgical + rehab care ➝ mobility and independence can be maintained.
✅ Conclusion
Fractured neck of femur is a major orthopaedic emergency, common in elderly patients with osteoporosis and falls. Intracapsular fractures are particularly high risk due to compromised blood supply ➝ AVN + non-union. Prompt surgical management (fixation or replacement), multidisciplinary orthogeriatric input, and effective rehab are key to improving survival and function.
📚 References
- Royal College of Physicians – Fractured Neck of Femur
- NICE – Hip Fracture Management Guidelines
- Mayo Clinic – Hip Fracture
- UpToDate – Hip Fracture Overview
- British Orthopaedic Association – Hip Fracture Guidance