Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Juvenile Idiopathic Arthritis (Stills Disease)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: | Monoarticular Arthritis | Polyarticular Arthritis | Seronegative Spondyloarthropathies | Ankylosing Spondylitis | Enteropathic Spondyloarthritis | Reactive Arthritis | Psoriatic Arthritis
🧒 Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease of childhood. Aspirin should be avoided in children <12 due to the risk of Reye’s syndrome ⚠️. Tumour necrosis factor (TNF) 🧬 is a key pro-inflammatory cytokine in JIA pathogenesis.
📖 About
- Accounts for ~10% of all chronic arthritis in children.
- Onset usually <16 years (often <5 years).
- Systemic form may mimic infection or malignancy.
- Adult-onset Still’s disease is the adult equivalent, but rare.
🧬 Aetiology
- Equal male:female in systemic type; other subtypes more female.
- Genetic predisposition – HLA associations.
- Environmental triggers (infections, stress, trauma) may unmask disease.
- Pathogenesis: imbalance of Th1 (IFN-γ) and Th17 (IL-17) cells + dysregulated innate immunity (IL-1, IL-6, TNF-α).
🔑 Definitions
- Oligoarthritis: ≤4 joints in first 6 months.
- Polyarthritis: ≥5 joints in first 6 months.
- Systemic JIA (sJIA): Autoinflammatory form with fever + rash + organ involvement.
🌈 Subtypes
- Oligoarthritis – 50–60%.
- RF+ polyarthritis – 11–28% (resembles adult RA).
- RF– polyarthritis – 2–7%.
- Systemic JIA: 🩸 High spiking fevers, salmon-pink rash, lymphadenopathy, hepatosplenomegaly, serositis.
- Psoriatic arthritis 🎨.
- Enthesitis-related arthritis 🦶 – HLA-B27 associated.
- Undifferentiated arthritis.
🤒 Classic Clinical Features (Systemic JIA)
- Daily high fevers (>39°C), often evening spikes 🌡️.
- Transient pink/salmon maculopapular rash 🌸.
- Arthralgia/arthritis (sometimes late feature).
- Other: lymphadenopathy, hepatosplenomegaly, myocarditis, pericarditis, pleurisy, dry eyes (uveitis risk).
- ~50% risk of chronic destructive arthritis long-term 🦴.
🔎 Investigations
- Bloods: ↑ ESR, ↑ CRP, ↑ ferritin 📈 (esp. systemic JIA).
- FBC: Anaemia of chronic disease, ↑ neutrophils, ↑ platelets.
- Autoantibodies usually negative (ANA, RF, HLA-B27). ⚠️ High RF or ANA positivity may point to alternative diagnoses.
- Imaging: – X-rays may be normal early. – 🖥️ Ultrasound: synovial thickening, effusion, tenosynovitis. – MRI: 🥇 gold standard – detects bone marrow oedema and erosions.
🩺 Differentials
- Oligoarthritis mimics: Reactive arthritis, toxic synovitis, septic arthritis, osteomyelitis, haemophilia, sickle cell, trauma/NAT, tumours.
- Polyarthritis mimics: SLE, MCTD, rheumatic fever, IBD-related arthritis, sarcoid, CRMO.
- Systemic mimics: Infections (mycoplasma, EBV, endocarditis), Kawasaki disease, PFAPA, malignancy (ALL, lymphoma), autoinflammatory syndromes.
⚠️ Complications
- Growth disturbance & leg-length discrepancy.
- Joint contractures & disability.
- Macrophage activation syndrome (MAS) – life-threatening cytokine storm 🛑.
💊 Management
- All suspected JIA → urgent referral to paediatric rheumatology 👩⚕️.
- NSAIDs for pain & stiffness (avoid aspirin in <12).
- Steroids (systemic or intra-articular) for acute flares or organ involvement.
- Methotrexate – cornerstone steroid-sparing agent.
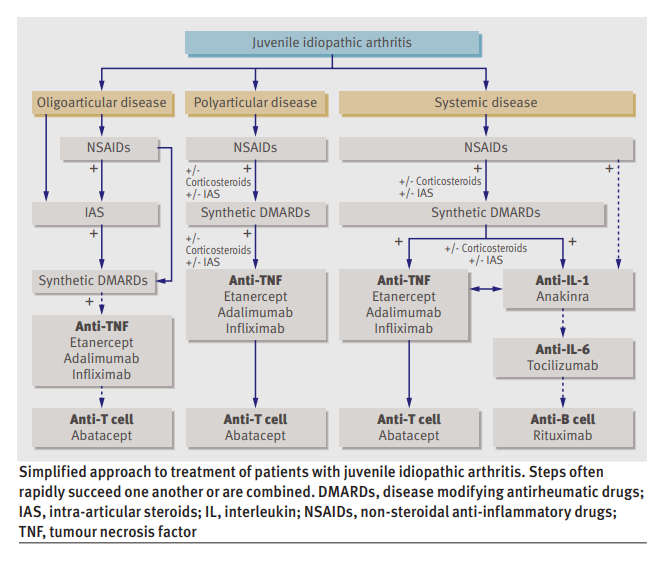
- Biologics: Anti-TNF (etanercept, adalimumab), IL-1 (anakinra), IL-6 (tocilizumab) for refractory cases 🧬.
- Vaccination: Avoid live vaccines if immunosuppressed. Annual flu 💉 recommended.
- Monitor growth, eye health (uveitis risk), and bone health (steroids + inactivity risk).
📚 References
Case – Systemic Juvenile Idiopathic Arthritis (Still’s disease)
A 9-year-old presents with 2 weeks of daily quotidian fevers peaking late afternoon, an evanescent salmon-pink rash appearing with fever, migratory arthralgia now localising to both knees, and sore throat; exam shows hepatosplenomegaly and mild lymphadenopathy. Labs: markedly ↑CRP/ESR, neutrophilia, anaemia, thrombocytosis, and very high ferritin (low glycosylated fraction if tested); cultures negative; CXR normal. After excluding infection and malignancy, diagnose systemic JIA; screen vigilantly for macrophage activation syndrome (MAS) (cytopenias, rising ferritin with falling ESR, ↑ALT, ↑triglycerides). Management: start systemic glucocorticoids for control and escalate early to targeted therapy—IL-1 blockade (anakinra) or IL-6 blockade (tocilizumab)—with physiotherapy and bone/gastroprotection; involve paediatric rheumatology and monitor joints, growth, LFTs, and MAS red flags.