Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
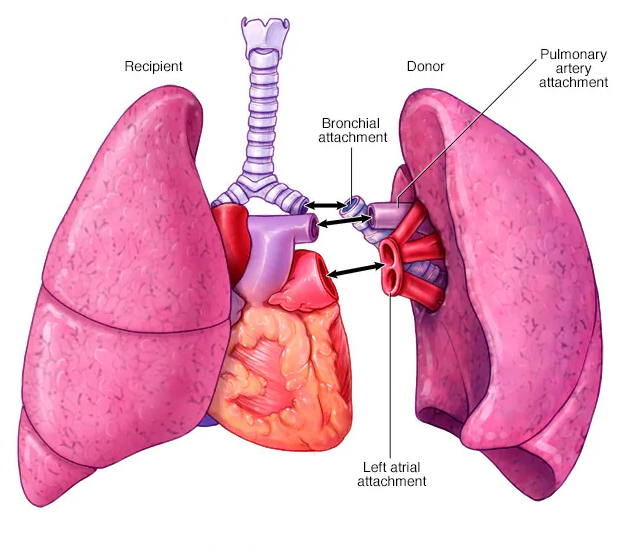
Lung Transplant
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Herpes Varicella-Zoster (Shingles) Infection
|Chickenpox Varicella Infection
|Varicella Cerebral Vasculopathy
|Herpes Viruses
|Herpes Zoster Ophthalmicus (HZO) Shingles
|MonkeyPox
|Mumps
|Measles
|Rubella (German Measles)
|Epstein-Barr Virus infection
|Cytomegalovirus (CMV) infections
|CMV retinitis infections
|Toxoplasmosis
💡 Key Point: Lung transplantation is life-saving for end-stage lung disease but carries high risks of infection, rejection, and long-term complications due to lifelong immunosuppression.
📖 About
🫁 Types
🎯 Indications
⚠️ Complications
🩺 Post-Transplant Care
📊 Prognosis
📚 References
3 Clinical Cases — Lung Transplantation 🫁🔄