Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Epidural Spinal abscess
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Transverse myelitis |Acute Disseminated Encephalomyelitis |Cervical spondylosis |Spinal Cord Anatomy |Acute Disc Prolapse |Spinal Cord Compression |Spinal Cord Haematoma |Foix-Alajouanine syndrome |Cauda Equina |Conus Medullaris syndrome |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome
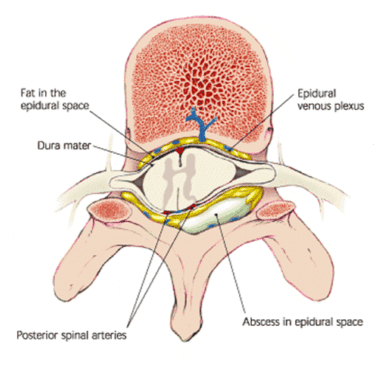
🧠 A spinal epidural abscess (SEA) is a rare but life-threatening infection in the epidural space, between vertebrae and dura mater. ⚡ It can rapidly compress the spinal cord → causing severe neurological deficits, paralysis, or death if untreated.
📖 About
- 🔴 Presents with severe back pain ± progressive weakness in legs/arms over hours–days.
- 🦠 Staphylococcus aureus (incl. MRSA) = most common pathogen.
- 🩸 Infection usually spreads haematogenously; may also extend from nearby bone/soft tissue or follow surgery.
- ⚠️ Classical triad = back pain + fever + neurological deficit (but only present in 10–15% at diagnosis).
🔬 Aetiology
- Haematogenous spread: Skin infection, UTI, endocarditis.
- Direct extension: Vertebral osteomyelitis, psoas abscess.
- Post-procedure: Spinal surgery, epidural catheterisation, nerve blocks.
- Trauma: Penetrating injury or open wound.
⚡ Risk Factors
- Diabetes mellitus.
- IV drug use 💉.
- Immunosuppression (HIV, steroids, chemo, transplant).
- Chronic kidney disease, alcoholism.
- Recent spinal surgery or invasive spinal procedure.
🩺 Clinical Presentation
- 🌡 Severe localised back pain, spinal tenderness.
- 🤒 Fever, malaise, sepsis signs.
- ⚡ Progressive motor/sensory deficits → paraparesis, quadriparesis, sensory level.
- 🚽 Autonomic dysfunction: bladder/bowel disturbance.
🚨 Red Flags
- Rapidly worsening weakness or paralysis.
- High fever, septic shock features.
- Recent spinal surgery or procedure.
- History of IV drug use or immunosuppression.
🧪 Investigations
- 🖥 MRI spine with contrast: Gold standard — defines abscess extent, cord compression.
- 🧬 Blood cultures: Often positive for S. aureus.
- 📊 Bloods: Raised CRP, ESR, WCC (inflammatory response).
- 🩻 CT spine: Alternative if MRI contraindicated (less sensitive for soft tissue).
🚨 SEA is a neurosurgical emergency. Delay in diagnosis/treatment greatly increases risk of permanent paralysis or death.
💊 Management
- Empirical IV Antibiotics: Start broad-spectrum (incl. MRSA cover e.g., vancomycin + ceftriaxone) → refine once cultures available. ⚠️ In unstable septic patients → do not delay antibiotics for imaging.
- Surgical Drainage: Laminectomy or CT-guided aspiration to relieve compression & obtain cultures.
- Supportive Care: Pain relief, neuro monitoring, bladder/bowel care, VTE prophylaxis, rehab for residual deficits.