Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Methanol Toxicity
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Drug Toxicity - clinical assessment |Metabolic acidosis |Aspirin or Salicylates toxicity |Ethylene glycol toxicity |Ethanol toxicity |Methanol toxicity |Ricin toxicity |Carbon Tetrachloride Toxicity |Renal Tubular Acidosis |Lactic acidosis |Iron Toxicity |Tricyclic Antidepressant Toxicity |Opiate Toxicity |Carbon monoxide Toxicity |Benzodiazepine Toxicity |Paracetamol (Acetaminophen) toxicity |Amphetamine toxicity |Beta Blocker toxicity |Calcium channel blockers toxicity |Cannabis toxicity |Cyanide toxicity |Digoxin Toxicity |Lithium Toxicity |NSAIDS Toxicity |Ecstasy toxicity |Paraquat toxicity |Quinine toxicity |SSRI Toxicity |Theophylline Toxicity |Organophosphate (OP) Toxicity |Toxin elimination by dialysis |Drug Toxicity with Specific Antidotes
🧪 Alcohol dehydrogenase inhibition is the cornerstone of methanol toxicity treatment. Antidotal therapy — with fomepizole or, if unavailable, ethanol — must be initiated immediately to prevent conversion of methanol into its toxic metabolites, formaldehyde and formic acid. Delay in antidote administration is the single biggest predictor of blindness and death.
📖 About
- Methanol poisoning is a classic example of a treatable toxic metabolic acidosis — it presents with a high anion and osmolar gap and characteristic visual and CNS toxicity.
- Outbreaks occur after ingestion of illicit alcohol (“moonshine”) or adulterated spirits, or through exposure to industrial solvents (e.g., antifreeze, cleaning fluid).
- Even a few millilitres can be lethal: as little as 10 mL may cause blindness; 30 mL can be fatal.
🧬 Aetiology & Pathophysiology
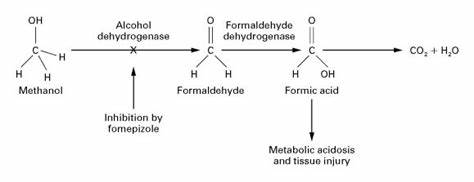
- Methanol itself is relatively inert until metabolised by hepatic enzymes.
- Step 1: Methanol → (via Alcohol Dehydrogenase, ADH) → Formaldehyde.
- Step 2: Formaldehyde → (via Aldehyde Dehydrogenase) → Formic Acid.
- Formic acid is a mitochondrial toxin that inhibits cytochrome oxidase → impaired oxidative phosphorylation → severe lactic acidosis.
- It accumulates particularly in optic nerves and basal ganglia → visual loss and neurological injury.
- Half-life of formic acid ≈ 20 hours (longer in metabolic acidosis or renal failure).
🔍 Common Sources
- Windscreen washer fluid, antifreeze, solvents, model engine fuel.
- Illicit spirits or industrial alcohol substitutes.
- Laboratory methanol or contaminated ethanol-based products.
🧠 Clinical Presentation
- 🕐 Latent phase (6–24h): patient may appear intoxicated or mildly unwell.
- 🧍 Systemic: Headache, dizziness, nausea, vomiting, abdominal pain.
- 🫁 Respiratory: Deep, rapid “Kussmaul” breathing due to metabolic acidosis.
- 👁️ Ophthalmic: Blurred vision, photophobia, “snow field” vision, progressing to blindness (optic neuritis).
- 🧠 Neurological: Confusion, agitation, seizures, coma.
- 🧪 Late: Severe acidosis, renal failure, visual loss, or respiratory arrest.
🧾 Investigations
- Blood tests: FBC, U&E (look for AKI), LFT, calcium (↓), CK if rhabdomyolysis suspected.
- ABG: Metabolic acidosis with raised anion gap (≥16 mmol/L).
- Osmolar gap: Elevated (>10–15 mOsm/kg) — early diagnostic clue before acidosis develops.
- Lactate: Falsely elevated due to formate interference in analyzers.
- Methanol level: Confirmatory but rarely available quickly — do not delay antidote.
- Urinalysis: May show calcium oxalate crystals (if mixed ethylene glycol ingestion).
- Imaging: CT/MRI: bilateral basal ganglia necrosis (putaminal lesions) in delayed cases.
📉 Key Diagnostic Triad
- 1️⃣ High anion gap metabolic acidosis
- 2️⃣ Raised osmolar gap
- 3️⃣ Visual or neurological symptoms
⚕️ Management Overview
Immediate priorities: Resuscitate → Antidote → Correct acidosis → Dialyse → Supplement folate
🏥 1. Immediate Stabilisation
- Secure airway, breathing, and circulation (ABCs).
- Administer oxygen (target SpO₂ 94–98%).
- IV fluids to maintain perfusion and enhance renal clearance.
- Monitor glucose — hypoglycaemia is common.
- Insert urinary catheter if oliguric; assess fluid output.
🧪 2. Antidotal Therapy
- Goal: Inhibit alcohol dehydrogenase to stop toxic metabolite formation.
- Fomepizole (preferred):
- Loading: 15 mg/kg IV over 30 min.
- Maintenance: 10 mg/kg every 12 h × 4 doses, then 15 mg/kg every 12 h until methanol <20 mg/dL, pH normalised, and asymptomatic.
- During haemodialysis: give same dose every 4 h (it is dialysable).
- Ethanol (if fomepizole unavailable):
- 5% solution: 15 mL/kg loading, then 2 mL/kg/h maintenance.
- 10% solution: 7.5 mL/kg loading, then 1 mL/kg/h maintenance.
- 40% spirits (emergency oral): 2 mL/kg loading, then 0.25 mL/kg/h.
- Double infusion rate for chronic alcohol users (enzyme induction).
- Therapeutic blood ethanol level: 100 mg/dL (22 mmol/L).
🧫 3. Correct Metabolic Acidosis
- Administer IV sodium bicarbonate if pH <7.25 or HCO₃⁻ <15 mmol/L.
- Monitor venous pH, K⁺, and lactate.
- Target pH >7.3 to improve formate metabolism.
🧬 4. Enhance Elimination
- Haemodialysis: Rapidly removes methanol, formate, and corrects acidosis.
- Indications:
- pH <7.25 or HCO₃⁻ <10
- Visual symptoms or coma
- Serum methanol >50 mg/dL (15 mmol/L)
- Renal failure or rising creatinine
- Continue until methanol undetectable and acidosis resolves.
🌿 5. Cofactor Therapy
- Folinic acid (Leucovorin): 50 mg IV/PO every 4–6 h for 24–48 h. → Accelerates formate metabolism to CO₂ and water.
- If folinic acid unavailable: give Folic acid 50 mg IV or 10 × 5 mg tablets orally.
- Thiamine (100 mg IV) and pyridoxine (50 mg IV) are added if ethylene glycol ingestion possible.
⚠️ 6. Monitoring
- Repeat ABG, osmolar gap, and electrolytes every 2–4 hours.
- Monitor vision daily — irreversible damage may occur within 24 h.
- Maintain careful fluid balance; watch for pulmonary oedema if large fluid loads given.
🧩 Treatment Summary Table
| Parameter | Treatment Approach | Notes |
|---|---|---|
| pH >7.2, HCO₃⁻ >20 | Observation ± oral ethanol | Mild poisoning; observe ≥24 h |
| pH 7.0–7.2, HCO₃⁻ 10–20 | Bicarbonate + ethanol/fomepizole ± dialysis | Moderate toxicity |
| pH <7.0 or HCO₃⁻ <10 | Bicarbonate + fomepizole + dialysis + folate | Severe, life-threatening |
🚫 Contraindications
- No absolute contraindication to antidote therapy — delay is more harmful.
- Relative: known allergy to fomepizole (use ethanol instead).
💊 Common Side Effects of Antidotes
- Ethanol: Hypoglycaemia, CNS depression, hypotension.
- Fomepizole: Headache, mild rash, transient ↑ liver enzymes, injection-site irritation.
📚 References
- Methanol Intoxication: Diagnostic and Treatment Approach. Am J Kidney Dis 2016.
- Methanol Poisoning Information (Methanol Institute)
- TOXBASE: Methanol and Ethylene Glycol Management Guidelines
- Brent J. “Fomepizole for Toxic Alcohol Poisoning.” N Engl J Med 2009;360:2216–2223.