Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Acute Coronary: Percutaneous Coronary Intervention
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular Infarction
⚠️ Always consult cardiology before discontinuing antiplatelet therapy after stent insertion. 🚫 Stopping clopidogrel or other antiplatelets too early (especially with drug-eluting stents) risks catastrophic in-stent thrombosis. 🕐 Standard practice: Dual Antiplatelet Therapy (DAPT) — aspirin + clopidogrel/ticagrelor/prasugrel — for 6–12 months, with aspirin often lifelong. 👉 Local / guideline variations exist, so confirm with the cardiology team.
ℹ️ About
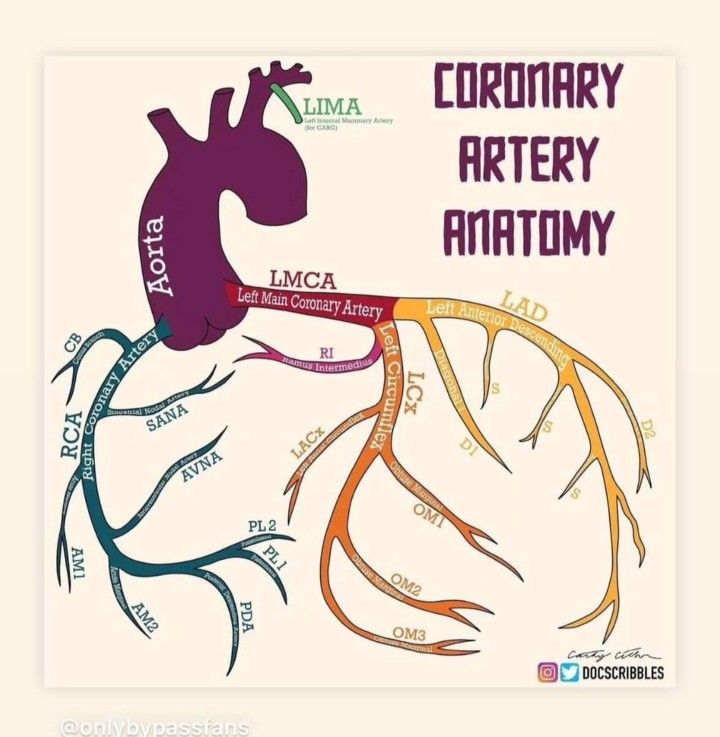
- PCI (Percutaneous Coronary Intervention): Opens blocked coronary arteries using balloons and stents to restore perfusion. Improves angina symptoms and quality of life, though elective PCI does not significantly reduce overall mortality.
- Originally developed to select candidates for CABG, PCI is now a primary treatment for many acute coronary syndromes (ACS).
- Widespread catheterization labs, even in district hospitals, allow rapid reperfusion without immediate need for cardiac surgery backup.
🧩 Stents
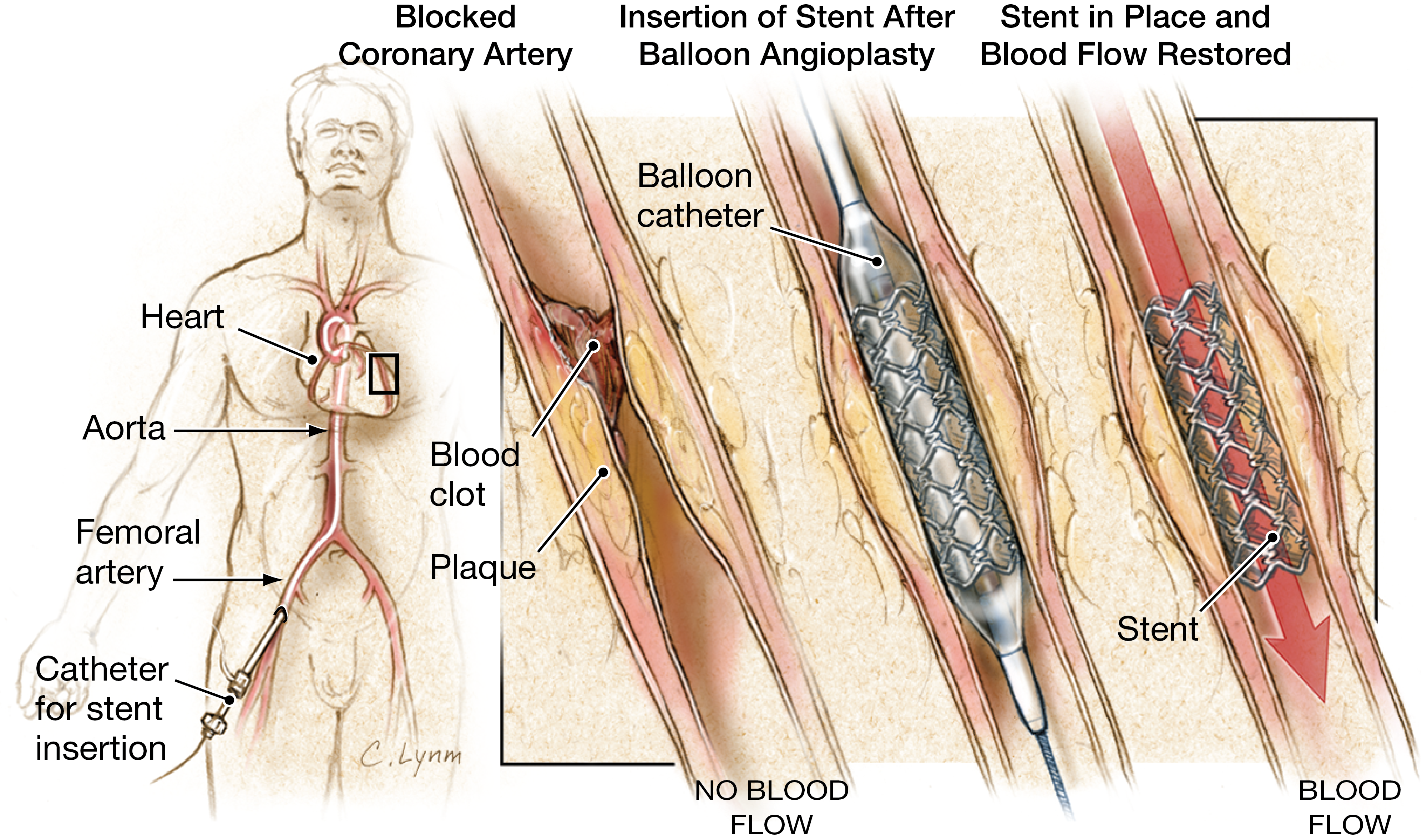
- 🛠️ Stents = metallic scaffolds to keep an artery open after balloon angioplasty.
- 🚑 Deployed via femoral or radial approach using guidewires and balloons under fluoroscopy.
- 💊 Drug-Eluting Stents (DES): Coated with antiproliferative drugs (e.g., sirolimus, paclitaxel) to reduce restenosis risk. Preferred in diabetics and complex lesions.
- ⚡ Difficult lesions: Long, calcified, eccentric, bifurcation, thrombotic, or tortuous arteries.
- 🩸 DAPT: Almost all patients receive aspirin + clopidogrel (or ticagrelor/prasugrel) for 6–12 months after PCI.
🏥 Indications (Mortality Benefit)
- 🚨 STEMI: Primary PCI within 90 minutes of first medical contact.
- 🚑 STEMI with hemodynamic compromise or failed thrombolysis.
- ⚡ STEMI in thrombolysis-contraindicated patients (e.g., recent intracranial hemorrhage).
📋 Other Indications
- High-risk NSTEMI.
- Unstable angina with high-risk features.
- Unexplained ischemic cardiomyopathy.
- Survivors of cardiac arrest where ischemia is suspected.
- Significant ventricular arrhythmias (VT) due to ischemic substrate.
🔍 Vascular Access
- Common sites: Radial artery (preferred for lower bleeding risk), femoral artery, or brachial artery.
📝 Protocol
- 🖊️ Consent: Mortality risk ~0.1% for diagnostic angiography, higher with PCI complexity.
- 🩸 Pre-procedure checks: FBC, platelets, U&Es, renal function, glucose, and peripheral pulses.
- 💊 Consider acetylcysteine in renal impairment (contrast nephropathy prevention — though evidence is mixed).
- 🚫 Fast for 6 hours, continue aspirin, load clopidogrel/ticagrelor as advised.
⚙️ Interventions
- 🎈 Balloon Angioplasty: Rarely used alone; risk of restenosis high.
- 🧱 Bare Metal Stents (BMS): Reduce restenosis vs balloon, but higher thrombosis risk. Shorter DAPT course than DES.
- 💊 Drug-Eluting Stents (DES): Reduce neointimal hyperplasia and restenosis; require longer DAPT.
- 🔀 Referral for CABG: Triple-vessel disease or significant left main stem involvement.
⚠️ Post-Procedure Complications
- 💉 Bleeding: At access site or retroperitoneal (suspect if hypotension + tachycardia).
- 🦵 Limb Ischemia: Cold, pale leg from thrombosis or dissection → urgent vascular review.
- 📈 Acute Stent Thrombosis: Presents like STEMI → urgent repeat PCI.
- 💧 Contrast Nephropathy: Monitor U&Es, hydrate well.
- 🧠 Stroke: Rare but serious embolic complication.
- 🦠 Infection / pseudoaneurysm / AV fistula: At puncture site, confirmed by ultrasound.
📚 Exam Tip: 👉 Always mention DAPT duration when discussing PCI. 👉 Drug-eluting stents reduce restenosis but require longer antiplatelet therapy. 👉 Radial access = fewer bleeding complications vs femoral.