Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Wilson disease
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Chronic liver disease |Cirrhosis |Alkaline phosphatase (ALP) |Liver Function Tests |Ascites Assessment and Management |Budd-Chiari syndrome |Autoimmune Hepatitis |Primary Biliary Cirrhosis |Primary Sclerosing Cholangitis |Wilson disease |Hereditary Haemochromatosis |Alpha-1 Antitrypsin (AAT) deficiency |Non alcoholic steatohepatitis (NASH) |Spontaneous Bacterial Peritonitis |Alcoholism and Alcoholic Liver Disease
Wilson's disease accounts for 6–12% of all acute liver failure cases referred for emergency liver transplantation. It should be suspected in any patient with unexplained liver disease or movement disorders of uncertain cause. Age alone must not be used to exclude the diagnosis.
📖 About
- Wilson’s disease is an autosomal recessive disorder of copper metabolism.
- Prevalence ~1 in 30,000 live births; carrier frequency ~1 in 90.
- Untreated → progressive copper accumulation in the liver, brain, cornea, and kidneys, leading to cirrhosis, neuropsychiatric decline, and early death.
- Early recognition and treatment are life-saving.
🧬 Aetiology
- Mutations in the ATP7B gene on chromosome 13 → defective copper-transporting ATPase.
- Defect prevents copper excretion into bile and incorporation into caeruloplasmin.
- Over 200 ATP7B mutations have been identified worldwide.
Kayser–Fleischer rings (copper in Descemet’s membrane of the cornea) are a hallmark feature. Best seen on slit-lamp exam, but not entirely specific.
🩺 Clinical Features
- Onset typically between ages 5–45.
- Hepatic: hepatitis, cirrhosis, hepatosplenomegaly, jaundice, acute liver failure.
- Haematological: Coombs-negative haemolytic anaemia (free copper damages RBC membranes).
- Neurological: dysarthria, dystonia, rigidity, tremor, choreoathetosis (due to basal ganglia copper).
- Ophthalmic: Kayser–Fleischer rings, sunflower cataracts (posterior lens surface).
- Psychiatric: irritability, poor impulse control, depression, psychosis.
- Musculoskeletal: osteoporosis, rickets from chronic disease.
🔍 Investigations
- Liver function: ↑ ALT/AST, prolonged PT in advanced disease.
- Haematology: Coombs-negative haemolysis.
- Biochemical markers:
- ↓ Serum caeruloplasmin (<0.2 g/L; <0.1 g/L highly specific).
- ↑ Free serum copper (>1.6 µmol/L).
- ↑ 24-hr urinary copper (>1.6 µmol/24h).
- ↑ Hepatic copper content (>250 µg/g dry weight).
- Ophthalmology: Slit lamp for Kayser–Fleischer rings.
- Renal: Tubular dysfunction → proteinuria, glycosuria.
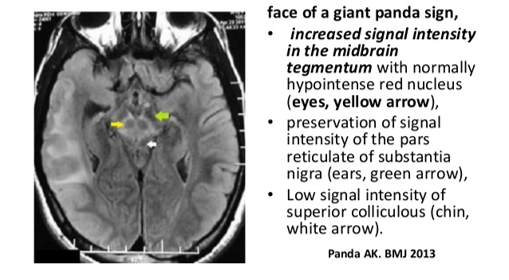
- MRI brain: basal ganglia/cerebellar changes, “giant panda sign”.
- Genetics: ATP7B mutation testing confirms but complicated by heterogeneity.
The combination of Kayser–Fleischer rings + low caeruloplasmin (<0.1 g/L) is diagnostic.
💊 Management
- Untreated Wilson’s disease is universally fatal.
- Copper chelation:
- D-penicillamine = first-line (but can cause lupus-like syndrome, nephrosis).
- Always give Pyridoxine (B6) with penicillamine.
- Trientine (triethylene tetramine) as alternative chelator.
- Zinc acetate: blocks intestinal copper absorption; safe for maintenance therapy.
- Dietary copper restriction (avoid shellfish, nuts, chocolate, mushrooms, liver).
- Liver transplantation: curative in fulminant hepatic failure or advanced cirrhosis.