Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Neonatal meningitis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
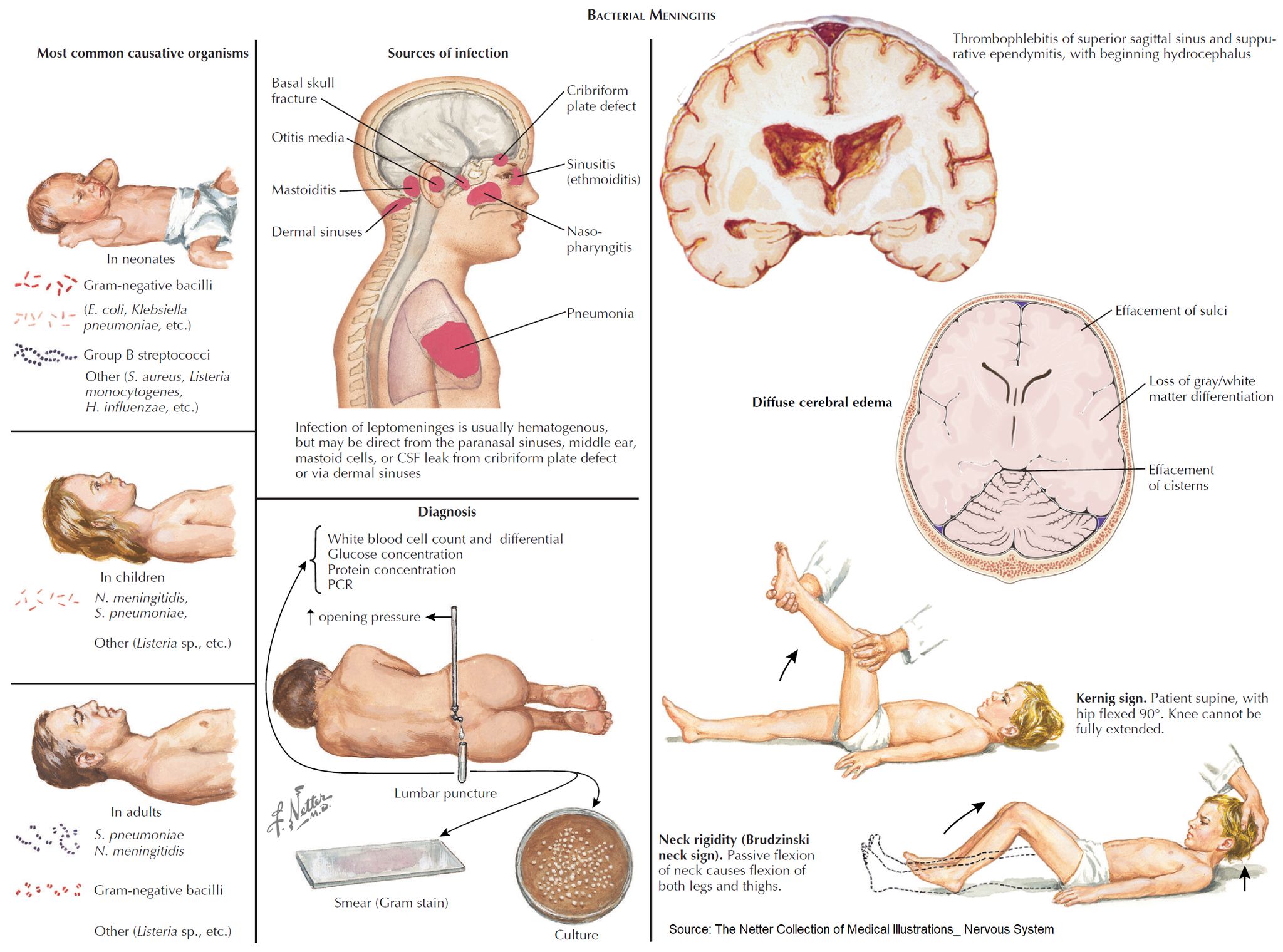
👶🧠 Neonatal meningitis – Definitive diagnosis is made by CSF examination via lumbar puncture (LP). LP should be performed in any neonate suspected of sepsis/meningitis, but ⚠️ treatment must not be delayed while awaiting results.
📖 About
- Occurs within the first 90 days of life 🍼.
- Most often bacterial, and is a life-threatening emergency 🚨.
🩺 Clinical Presentation
- ⚠️ Classical triad (fever, stiff neck, vomiting) often absent.
- Instead look for:
- ❌ Poor feeding, irritability, lethargy
- 😴 Apnoea, listlessness, reduced tone
- 🌡️ Fever OR hypothermia
- ⚡ Seizures
- 🚩 Other red flags: bulging fontanelle, high-pitched cry, hypoglycaemia, metabolic acidosis, shock, pallor
🦠 Microbiology
- Group B Streptococcus (GBS) 🧬 → ~50% (esp. type III; vertical transmission).
- Escherichia coli (K1 capsule) 🦠 → ~20%.
- Listeria monocytogenes 🥗 → 5–10% (contaminated food in pregnancy).
- Viruses 🦠 → HSV, VZV (less common, but important for prognosis).
⚠️ Complications
- ♿ Cerebral palsy (~8%)
- 📘 Learning disability (~7%)
- ⚡ Persistent seizures (~7%)
- 👂 Hearing loss (~25%)
- 🧠 Hydrocephalus, abscess, or subdural effusion
👶➡️👧 Causes in Older Infants (>3 months)
- Streptococcus pneumoniae 🧬
- Neisseria meningitidis 💉
- Haemophilus influenzae type b (Hib) 💊 (much less common since vaccination).
💊 Management
- 🚑 Immediate IV antibiotics (before LP if unstable):
- Ampicillin + Cefotaxime (UK NICE guidance) 💉
- Avoid ceftriaxone in neonates (risk of kernicterus) ❌
- 💧 Supportive care: fluids, oxygen, seizure control (phenobarbital/levetiracetam).
- 🦠 If HSV suspected: add Acyclovir 🧪
- 🔊 Hearing test follow-up (due to high risk of deafness).
- 🧪 Close monitoring: blood cultures, CSF studies, CRP trends.
- 👩👦 Public health: maternal screening & prophylaxis for GBS at delivery reduces risk.
🧑🏫 Exam Tip
Neonatal meningitis is one of the few conditions where the common organisms differ significantly from older children. Always think GBS, E. coli, and Listeria 👶 — whereas after 3 months, pneumococcus and meningococcus dominate.
Cases — Neonatal Meningitis
- Case 1 — Early-onset GBS infection 🍼: A 3-day-old term infant presents with poor feeding, irritability, and fever. Exam: bulging fontanelle, lethargy. CSF: neutrophilia, low glucose, high protein. Blood culture: Group B Streptococcus. Diagnosis: early-onset neonatal meningitis (GBS). Managed with IV benzylpenicillin + gentamicin, then tailored antibiotics.
- Case 2 — E. coli meningitis 🦠: A 10-day-old preterm baby develops temperature instability, seizures, and poor tone. Mother had prolonged rupture of membranes. CSF: Gram-negative bacilli, low glucose, high protein. Culture: E. coli K1. Diagnosis: neonatal meningitis due to E. coli. Managed with IV cefotaxime for 21 days.
- Case 3 — Listeria infection 🥛: A 14-day-old infant presents with poor feeding, apnoea, and irritability. Mother ate unpasteurised cheese during pregnancy. CSF: mononuclear predominance, positive Gram-positive bacilli. Diagnosis: Listeria monocytogenes meningitis. Managed with IV ampicillin + gentamicin.
Teaching Point 🩺: Neonatal meningitis is most often caused by Group B Strep, E. coli, or Listeria. - Early onset (<7 days): GBS, E. coli, Listeria (maternal transmission). - Late onset (>7 days): same organisms + nosocomial Gram-negatives. Presents non-specifically (poor feeding, irritability, temperature instability, seizures). Management: urgent IV antibiotics + supportive care. Mortality and neurological sequelae remain high.