Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Acute Glaucoma
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Episcleritis |Scleritis |Assessing a Red eye |Acute Angle Closure Glaucoma |Allergic and Infective Conjunctivitis |Anterior and Posterior Uveitis |Herpes simplex keratitis (HSK)
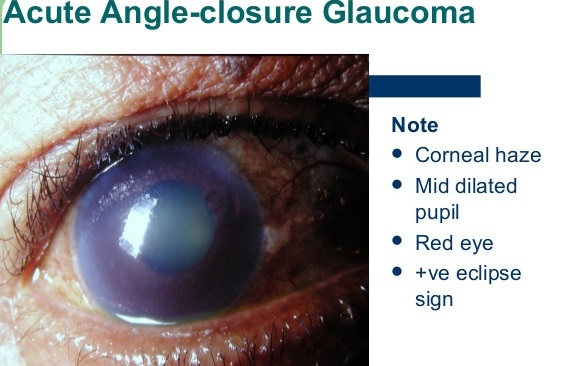
Acute Angle Closure Glaucoma (AACG) is a true ophthalmic emergency 🚨. A sudden rise in intraocular pressure (IOP) causes severe ocular pain, visual loss, and systemic upset. If untreated, optic nerve damage and permanent blindness may occur within hours to days.
📖 About
- Caused by pupillary block in predisposed eyes with shallow anterior chambers → iris bows forward → blocks aqueous outflow.
- Often triggered by pupillary dilation (dim light 🌙, stress, drugs such as anticholinergics or sympathomimetics).
- Rare after cataract surgery (lens removal deepens the chamber).
- “Golf ball hardness” globe on palpation = classic bedside clue.
- More common in older females (narrower anterior chambers).
🧬 Aetiology & Pathophysiology
- Pupillary block: aqueous humour cannot pass through pupil → pressure gradient pushes iris forward → trabecular meshwork blocked → IOP rises.
- Precipitating factors:
- Dim light → physiological mydriasis.
- Drugs: anticholinergics (atropine, tricyclics), sympathomimetics (decongestants), topiramate.
- Emotional stress.
- Prolonged high IOP → ischaemic optic neuropathy → irreversible vision loss.
📊 Epidemiology
- Incidence: ~1 in 1,000 White, 1 in 100 Asian, up to 4 in 100 Inuit populations.
- Age: typically >60 years.
- Sex: female > male (~4:1).
- Risk factors: hyperopia, family history, shallow anterior chamber (short axial length).
🩺 Clinical Features
- ⚡ Sudden severe ocular pain + headache.
- 🌈 Blurred vision, halos around lights.
- 👁️ Red eye with mid-dilated, fixed pupil.
- 🥴 Nausea, vomiting, systemic upset (can mimic GI pathology).
- 🌫️ Corneal edema (“steamy cornea”).
- IOP usually >40 mmHg (normal 10–21).
🔎 Differential Diagnosis of a Painful Red Eye
| Condition | Features | Distinguishing Points |
|---|---|---|
| AACG | Sudden pain, halos, mid-dilated pupil, hazy cornea, hard globe | Systemic upset (nausea/vomiting), halos 🌈 |
| Anterior Uveitis | Pain, photophobia, small irregular pupil | Pupil constricted, no halos, responds to steroids |
| Keratitis | Red, gritty eye, photophobia | Contact lens use, fluorescein staining shows ulcer |
| Conjunctivitis | Red, sticky eye, mild discomfort | No vision loss, globe not hard |
🧪 Investigations
- Tonometry: IOP usually >40–70 mmHg.
- Slit-lamp: Corneal edema, shallow chamber, fixed pupil.
- Gonioscopy: Closed anterior chamber angle.
- Visual fields: For long-term glaucomatous damage monitoring.
🚑 Stepwise Management
- Immediate (ED/GP setting)
- IV Acetazolamide 500 mg stat (carbonic anhydrase inhibitor).
- Topical Timolol 0.5% (beta-blocker) – reduces aqueous production.
- Analgesia + antiemetics for distress.
- O₂ if hypoxic.
- Next (once IOP begins to fall)
- Pilocarpine 2% drops – miotic → pulls iris away from angle.
- IV Mannitol 20% if refractory to initial measures.
- Definitive
- Laser peripheral iridotomy (LPI) in affected + fellow eye (prophylaxis).
- Surgical iridectomy if LPI unavailable.
🧾 Clinical Pearls
- Any elderly patient with sudden red eye + vomiting → assume AACG until proven otherwise.
- Never dilate pupils if AACG is suspected ❌.
- Fellow eye must always be treated prophylactically with iridotomy.
- Digital palpation: AACG feels like a “rock-hard” eye 🎾.
🖼️ Key Illustrations

💡 Teaching Pearl: AACG is one of the few causes of a painful red eye with systemic upset. Always compare to anterior uveitis (small irregular pupil) and keratitis (corneal ulcer in contact lens wearers). Rapid recognition + immediate acetazolamide + ophthalmology referral = sight-saving intervention.
Cases — Acute Angle-Closure Glaucoma (AACG)
- Case 1 — Classic sudden attack 👁️: A 64-year-old woman presents with sudden severe right eye pain, blurred vision, and halos around lights. She has nausea and vomiting. Exam: red eye with hazy cornea, fixed mid-dilated pupil, hard globe. Intraocular pressure (IOP): 56 mmHg. Diagnosis: acute angle-closure glaucoma. Managed with immediate IV acetazolamide, topical beta-blocker, pilocarpine, and urgent ophthalmology referral for laser iridotomy.
- Case 2 — Triggered by dark environment 🌙: A 58-year-old man develops severe eye pain and headache after spending several hours in a cinema. Exam: conjunctival injection, cloudy cornea, fixed semi-dilated pupil. Diagnosis: AACG precipitated by pupillary dilation in dark. Managed with emergency IOP-lowering drops and definitive laser peripheral iridotomy to both eyes (prophylactic in fellow eye).
- Case 3 — Subacute/recurrent AACG ⚠️: A 62-year-old woman presents with intermittent blurred vision, halos, and mild ocular pain after reading for long periods. Episodes resolve spontaneously but recur. Exam between episodes: shallow anterior chamber, narrow drainage angle on gonioscopy. Diagnosis: subacute angle-closure glaucoma. Managed with prophylactic laser peripheral iridotomy to prevent a full-blown acute attack.
Teaching Point 🩺: AACG occurs when the trabecular meshwork is suddenly blocked by the iris, rapidly raising IOP. Symptoms: sudden eye pain, blurred vision, halos, headache, nausea/vomiting. Signs: red eye, hazy cornea, mid-dilated fixed pupil, hard globe, very high IOP. Risk factors: hypermetropia, older age, female sex, Asian ethnicity, pupillary dilation. Management: emergency IOP-lowering (acetazolamide, beta-blocker, pilocarpine, mannitol) and definitive laser iridotomy.