Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Multiple Myeloma
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Hypercalcaemia |Multiple Myeloma |Extramedullary Plasmacytoma |Smouldering Myeloma |MGUS |Waldenstrom Macroglobulinaemia |Oncological emergencies
🔎 Always think of myeloma in a patient with bone pain, raised calcium, or an unexplained high ESR.
📘 About
- Malignant tumour of plasma cells (B-cell lineage).
- Produces monoclonal immunoglobulin (usually IgG or IgA) or light chains (Bence–Jones proteins).
- Median survival ~2–3 years (improving with newer therapies).
📊 Incidence
- ~5,500 new cases per year in the UK 🇬🇧.
- Incidence ~5.4/100,000/year; more common in men.
- Twice as common in patients of African descent.
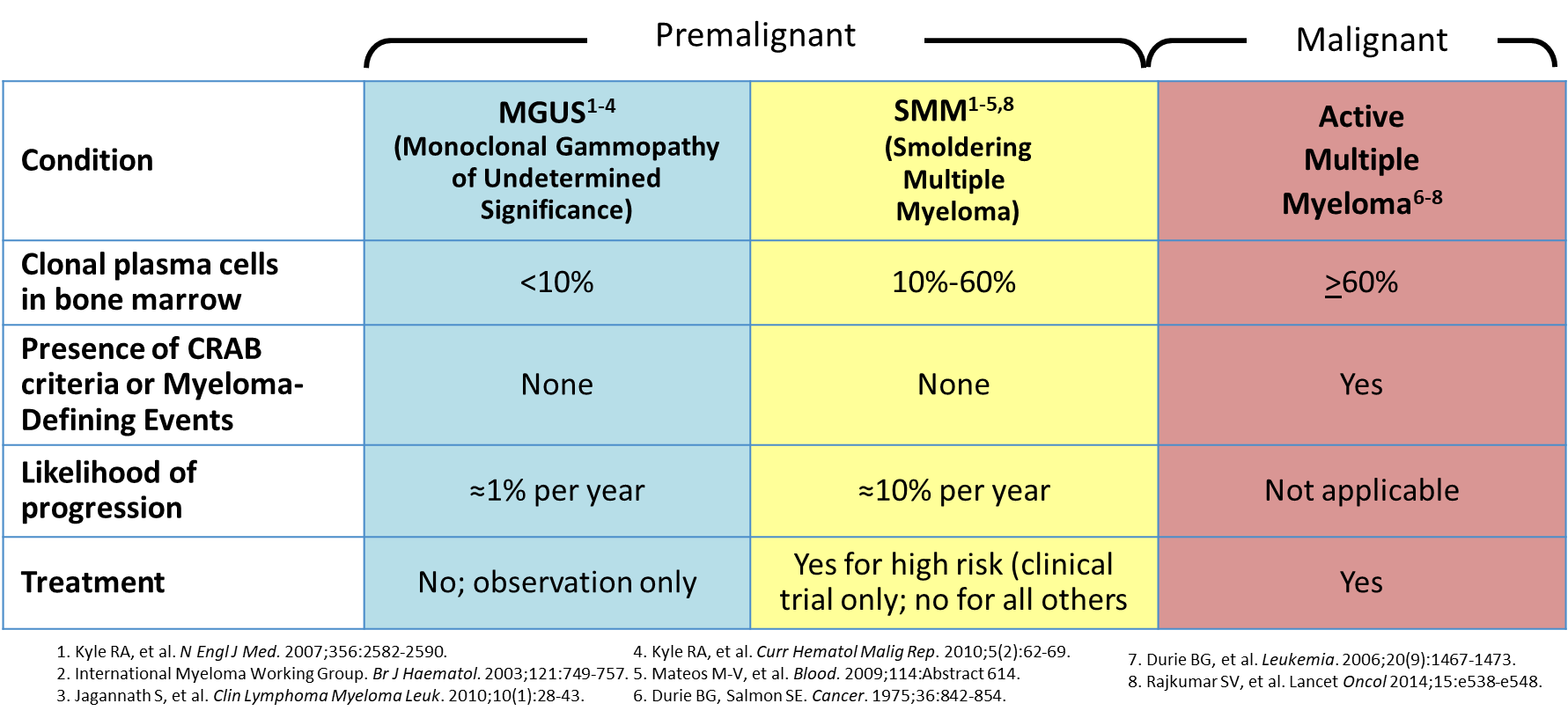
📈 Spectrum of Plasma Cell Disorders
- MGUS (Monoclonal Gammopathy of Undetermined Significance): Asymptomatic, low paraprotein, no organ damage. ~1% per year progress to myeloma. Managed with monitoring only 🩺.
- Smouldering Myeloma: Higher paraprotein and marrow plasma cells, but still no CRAB features. Requires close observation 👀.
- Multiple Myeloma: Full-blown disease with monoclonal protein + ≥1 CRAB feature (end-organ damage).
💡 CRAB = HyperCalcaemia, Renal impairment, Anaemia, Bone lesions.
⚙️ Aetiology & Pathophysiology
- Uncontrolled plasma cell clone infiltrates marrow → cytopenias.
- Secretion of abnormal immunoglobulins → hyperviscosity & renal failure.
- Suppression of normal immunoglobulins → immunodeficiency 🔻.
- Plasma cell proteins stimulate osteoclasts → lytic bone disease & fractures 🦴.
- Light chains damage kidneys → cast nephropathy.
🧑⚕️ Clinical Features
- Age >60, male > female.
- Bone pain (esp. back, ribs, skull); vertebral collapse → cord compression.
- Renal impairment (light chain nephropathy).
- Infections due to low normal immunoglobulins (immunoparesis).
- Anaemia → fatigue, pallor.
- Hypercalcaemia → thirst, confusion, constipation.
- AL Amyloidosis: neuropathy, restrictive cardiomyopathy, nephrotic syndrome, macroglossia 👅.
- Hyperviscosity syndrome (IgA myeloma): blurred vision, headaches, bleeding.
🧪 Investigations
- FBC: Normocytic anaemia, cytopenias.
- Biochemistry: ↑ ESR, ↑ calcium, ↑ urate, ↑ LDH.
- Renal function: may show AKI or CKD.
- Serum protein electrophoresis & urine for BJP: Monoclonal paraprotein.
- Bone marrow aspirate/biopsy: >10% clonal plasma cells; FISH for cytogenetics.
- Imaging: Whole-body MRI, CT or PET-CT for lytic lesions.
- Prognosis: β2-microglobulin ↑ = poor prognosis.
🩸 CRAB Mnemonic
- 🟠 Hypercalcaemia: Ca²⁺ >2.75 mmol/L.
- 🟣 Renal failure: CrCl <40 ml/min or creatinine >177 µmol/L.
- 🔴 Anaemia: Hb <100 g/L.
- ⚫ Bone lesions: lytic lesions, fractures, osteoporosis.
🚑 Complications
- Pathological fractures & spinal cord compression.
- Hypercalcaemia crisis.
- Renal failure (cast nephropathy).
- Recurrent infections (esp. pneumonia, sepsis).
- Pancytopenia & bleeding.
💊 Management
- Fit / Younger Patients: Bortezomib + thalidomide + dexamethasone → autologous stem cell transplant (ASCT).
- Supportive: Transfusions, bisphosphonates (zoledronate/pamidronate) for bone disease, hydration for hypercalcaemia.
- Pain management: Analgesics, radiotherapy for focal lesions.
- Hyperviscosity: Plasma exchange if symptomatic.
- Prophylaxis: Vaccinations, antibiotics, allopurinol for hyperuricaemia.
- Palliative: Discuss prognosis, goals of care, symptom management.
📌 Key exam pearl: If you see “elderly patient + back pain + renal impairment + hypercalcaemia + raised ESR” → think myeloma until proven otherwise 🚨.
Cases — Multiple Myeloma
- Case 1 — Bone pain & lytic lesions 🦴: A 68-year-old man presents with persistent back pain and fatigue. Exam: spinal tenderness. Bloods: normocytic anaemia, calcium 3.1 mmol/L, creatinine 160 µmol/L. X-ray: “punched-out” lytic lesions in vertebrae. Serum electrophoresis: monoclonal IgG spike. Diagnosis: multiple myeloma with bone disease. Managed with bisphosphonates, chemotherapy (bortezomib/lenalidomide/dexamethasone), and supportive care.
- Case 2 — Renal impairment 🩺: A 72-year-old woman is admitted with confusion and oliguria. Bloods: urea 25 mmol/L, creatinine 480 µmol/L, calcium 2.7 mmol/L. Urine: Bence–Jones proteinuria. Renal biopsy: light chain cast nephropathy. Diagnosis: myeloma kidney. Managed with hydration, chemotherapy, and dialysis if required.
- Case 3 — Recurrent infections 🦠: A 61-year-old man has recurrent pneumonias and sinusitis. Bloods: IgG low, Hb 9.5 g/dL, raised ESR. Serum electrophoresis: monoclonal IgA band. Bone marrow: 20% plasma cells. Diagnosis: multiple myeloma with immunoparesis. Managed with chemotherapy, immunoglobulin replacement, and infection prophylaxis.
Teaching Point 🩺: Multiple myeloma is a malignant plasma cell disorder producing monoclonal immunoglobulins. Classic features = CRAB: - Calcium ↑ (hypercalcaemia) - Renal impairment - Anaemia - Bone lesions Diagnosis requires serum/urine electrophoresis, free light chain assay, and bone marrow biopsy. Treatment = chemotherapy, bisphosphonates, and supportive care.