Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Granulomatosis with Polyangiitis GPA (Wegeners)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: Granulomatosis with Polyangiitis (GPA, formerly Wegener's) | Goodpasture's Syndrome (Anti-GBM Disease) | Respiratory Failure | Acute Kidney Injury
Early diagnosis and immunosuppression are key to reducing damage. If suspicious, get an urgent cANCA (proteinase 3). Without intervention, GPA can destroy kidneys within weeks.
ℹ️ About
- 🧑⚕️ First described by Dr. Friedrich Wegener in 1936 (renamed GPA due to his Nazi association).
- 📛 Now called Granulomatosis with Polyangiitis (GPA).
- 🩸 Systemic necrotizing vasculitis affecting ENT, lungs, kidneys.
- ⏱️ Untreated → 90% mortality within 2 years.
🧬 Aetiology & Pathophysiology
- 🌡️ Medium-sized vessel vasculitis, likely autoimmune/hypersensitivity to environmental antigen.
- 🦠 Staphylococcus aureus carriage linked to recurrence; eradication reduces relapse risk.
- 🩺 Renal involvement in 40% at presentation, up to 90% during disease course.
- 🪢 Granulomatous inflammation → necrosis of affected tissues.
📊 Epidemiology
- 👥 Incidence: ~3/100,000 (USA).
- ⏱️ Mean onset age ~50 yrs.
- ⚖️ M:F ratio = 1:1.
- 🌍 90% in Caucasian populations.
🧱 Granuloma Formation
🩺 Clinical Presentation
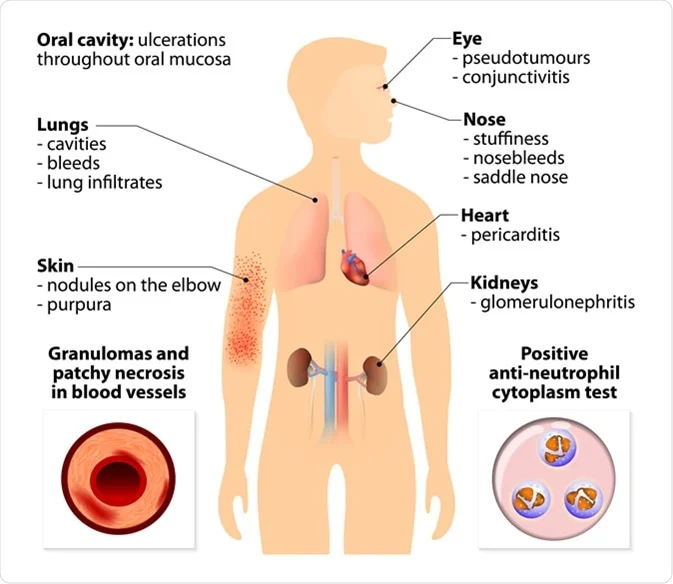
- 🛏️ Constitutional: Fever, night sweats, malaise, lethargy.
- 👃 ENT: Rhinorrhoea, epistaxis, sinusitis, otitis media, nasal septal perforation, saddle nose deformity.
- 🫁 Lungs: Cough, haemoptysis, pulmonary haemorrhage (↑DLCO), nodules ± cavitation.
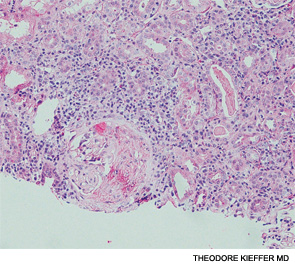
- 🧽 Kidneys: Hypertension, haematuria, pauci-immune necrotizing glomerulonephritis (hallmark lesion).
- 👁️ Ocular: Uveitis, scleritis, proptosis.
🔬 Investigations
- 🩸 FBC: Anaemia, leukocytosis.
- 🧪 U&E: Raised urea/creatinine → renal impairment.
- 🔥 Inflammatory markers: ↑ ESR/CRP.
- 🧪 Complement: Often low.
- 🫁 CXR: Nodules, infiltrates, cavitations, haemorrhage.
- 🧫 Urinalysis: Proteinuria, haematuria, dysmorphic RBCs, RBC casts.
- 🖥️ HRCT: Alveolar haemorrhage, nodules, airway stenosis.
- 🔑 ANCA: • cANCA (PR3) → positive in 80–90% (correlates with activity). • pANCA (MPO) → positive in 10–20%.
- 🔍 Biopsy: ENT/lung/renal tissue → necrotizing granulomatous inflammation.
- 🫁 BAL: Helpful in alveolar haemorrhage (blood in alveoli).
- 💨 DLCO: Raised in alveolar haemorrhage (Hb binding CO).
🖼️ CT Findings
📸 CT shows multiple cavitary (arrows) and non-cavitary (arrowheads) pulmonary nodules typical of GPA.

💊 Management
- ⚠️ Untreated mortality: 90% in 2 years. Treatment dramatically improves survival.
- Induction: • Severe disease → high-dose corticosteroids + Cyclophosphamide (CYC) or Rituximab (RTX). • Non-severe → Methotrexate (MTX) or Rituximab ± steroids.
- Maintenance: • Azathioprine, Methotrexate, or Rituximab (esp. PR3+ relapsers). • Rituximab infusions can be extended up to 42 months in high-risk relapse cases.
- Adjuncts: • Co-trimoxazole prophylaxis (for Pneumocystis jirovecii + reduces Staph. nasal colonisation). • Long-term mupirocin cream for Staph. carriage. • Plasma exchange (PLEX) for severe renal disease (Cr >500 μmol/L) or pulmonary haemorrhage.
📚 References
Case – Granulomatosis with Polyangiitis (GPA, Wegener’s)
A 42-year-old with months of chronic sinusitis, epistaxis, and conductive hearing loss presents with pleuritic chest pain, cough with blood-streaked sputum, fatigue, and new ankle oedema. Exam: saddle-nose deformity, crackles; BP 158/92. Labs: normocytic anaemia, creatinine rising, active urine sediment with RBC casts; CXR shows multiple cavitating nodules. Serology: c-ANCA (PR3) strongly positive. Urgent renal tract ultrasound is normal; CT chest confirms nodules; nasal/renal biopsy shows necrotising granulomatous vasculitis. Treat as organ-threatening AAV: IV methylprednisolone (then high-dose oral taper) plus rituximab (or cyclophosphamide) with PPI, bone protection, and PJP prophylaxis. Add plasmapheresis only if severe pulmonary haemorrhage or dialysis-dependent RPGN per local policy. Once in remission, maintain with rituximab/azathioprine; involve ENT, respiratory, nephrology; vaccinate and monitor for relapse and treatment toxicity. Differentials: microscopic polyangiitis, EGPA, TB/fungal infection, malignancy.