Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Wellens Syndrome
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |Acute Coronary Syndrome (ACS): Complications |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular STEMI |ACS: Sgarbossa Criteria |Wellen's syndrome
⚠️ Because Wellens syndrome patients have critical narrowing of the LAD coronary artery, stress testing is contraindicated. It may precipitate acute MI and sudden cardiac death.
🔎 Introduction
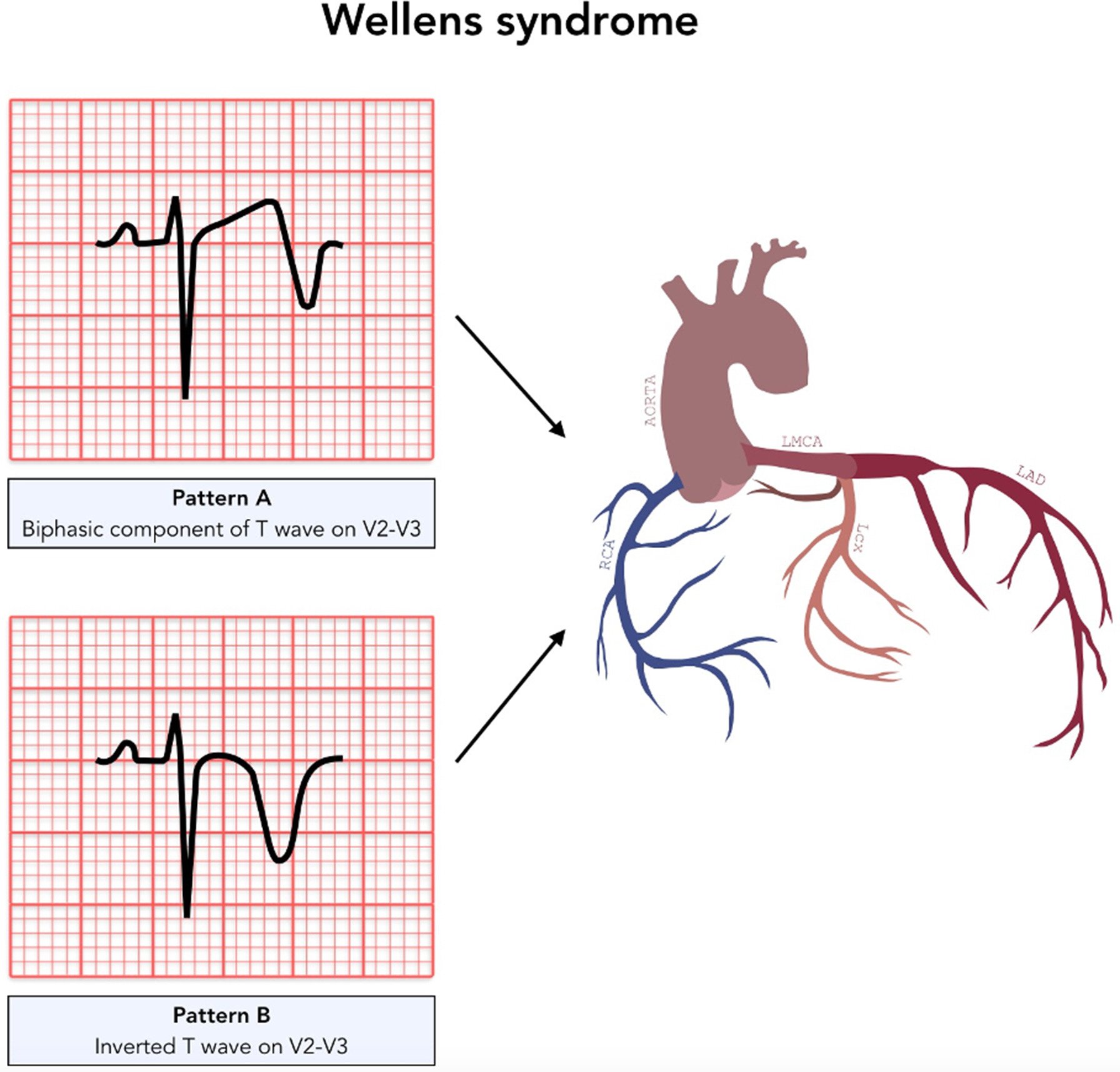
- Wellens syndrome = a classic ECG pattern indicating imminent anterior MI due to critical LAD stenosis.
- Key to recognise in the ED – early intervention is lifesaving.
🧬 Aetiology
- Represents >90% stenosis of the LAD artery.
- Critical narrowing → high risk of complete occlusion & anterior wall STEMI.
⚙️ Pathophysiology
- Atherosclerotic plaque: High-grade LAD lesion causes intermittent reduced perfusion.
- Vasospasm: LAD spasm may contribute to transient ischaemia.
- Increased demand: Exercise/stress raises oxygen demand, worsening ischaemia.
- Hypoxia: Systemic hypoxaemia aggravates LAD compromise.
⚠️ Risk Factors
- Diabetes mellitus
- Hypertension
- Hyperlipidaemia / Hypercholesterolaemia
- Smoking
- Metabolic syndrome
- Family history of premature IHD
- Age & occupational stress
🧾 Clinical Presentation
- Chest pain (often anginal, may have settled by time of ECG).
- Anginal equivalents: arm pain, jaw pain, dyspnoea.
- May be asymptomatic → ECG is crucial.
📊 Investigations
- Bloods: FBC, U&E, LFTs, lipids.
- Troponin: May be normal or only mildly raised.
- ECG hallmarks:
- Biphasic or deeply inverted T waves in V2–V3.
- Can extend V1–V6 (critical LAD territory).
- T wave normalisation + hyperacute waves = impending STEMI.
- Echocardiogram: Wall motion abnormalities in anterior wall.
- Coronary angiography: Gold standard for diagnosis & management planning.
🩺 Management
- Immediate Care: Admit CCU, oxygen if hypoxic, aspirin/clopidogrel, nitrates, beta-blockers (if not contraindicated).
- STEMI protocol: If ST elevation develops → manage as acute STEMI.
- Definitive: Early coronary angiography → PCI or CABG depending on anatomy.
- Avoid stress testing: Contraindicated due to risk of precipitating full infarct.
📌 Prognosis & Clinical Significance
- Untreated → very high risk of anterior wall MI within days to weeks.
- Early recognition + PCI/CABG = excellent outcome.
- Secondary prevention vital: BP & cholesterol control, diabetes optimisation, smoking cessation, antiplatelet + statin therapy.
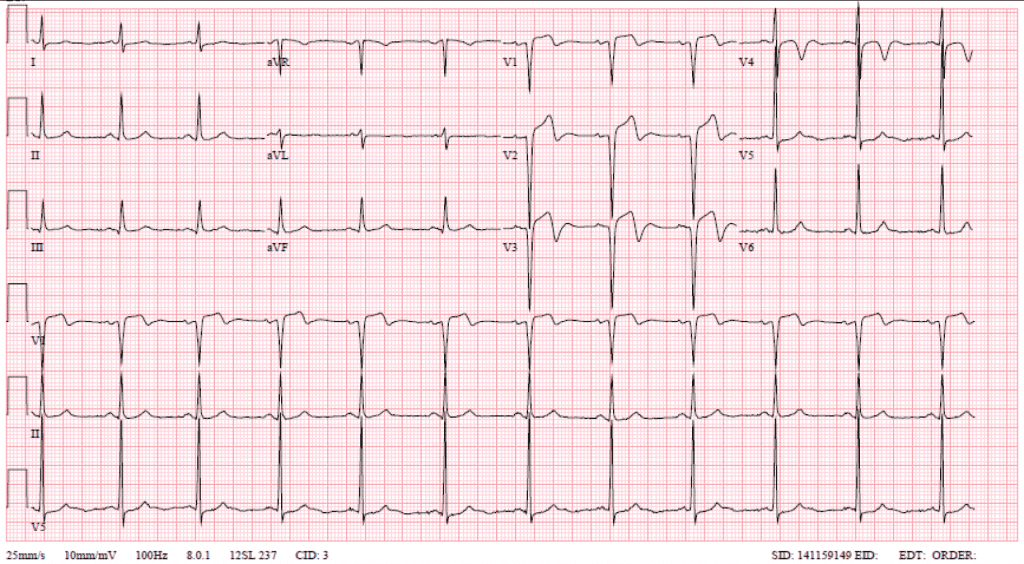
🖼️ Classic ECG Examples





📚 References
- Wellens Syndrome – NCBI Bookshelf
- de Zwaan C, Wellens HJ. “Characteristic electrocardiographic pattern indicating critical LAD stenosis.” Am Heart J. 1982.
Exam Pearl: – Wellens = T-wave changes in V2–V3 + critical LAD stenosis + pain-free at time of ECG. – Never stress test a Wellens patient 🚫🏃.
Cases — Wellens’ Syndrome
- Case 1 — Type A (biphasic T-waves) 📉: A 56-year-old man presents with intermittent central chest tightness over 2 days, now pain-free. ECG: biphasic T-waves in V2–V3, no ST elevation. Troponin mildly raised. Diagnosis: Wellens’ syndrome (critical LAD stenosis, Type A pattern). Managed with hospital admission, antiplatelets, and urgent coronary angiography ± PCI. ⚠️ Stress testing contraindicated due to risk of infarction.
- Case 2 — Type B (deeply inverted T-waves) ⚠️: A 63-year-old woman with diabetes presents with recent exertional angina, now pain-free in ED. ECG: deeply inverted, symmetrical T-waves in V2–V4, preserved R-wave progression. Troponin borderline. Diagnosis: Wellens’ syndrome (Type B pattern). Managed with dual antiplatelet therapy, heparin, and urgent revascularisation planning.
- Case 3 — Missed diagnosis → infarction 🚨: A 60-year-old man is discharged after presenting with atypical chest pain and “nonspecific T-wave changes.” Two days later he returns with severe chest pain. ECG: anterior ST-elevation MI. Angiography: complete proximal LAD occlusion. Retrospective review: prior ECG showed Wellens’ T-wave inversions. Diagnosis: progression of untreated Wellens’ syndrome to LAD infarction. Teaching point: always recognise the pattern!
Teaching Point 🩺: Wellens’ syndrome is a pre-infarction state caused by critical proximal LAD stenosis. ECG patterns (seen in pain-free state): - Type A: biphasic T-waves in V2–V3. - Type B: deeply inverted, symmetrical T-waves in anterior leads. No Q waves, no loss of R-wave progression, little ST elevation. ⚠️ High risk of extensive anterior MI → requires urgent angiography/PCI, not stress testing. Troponin may be normal or only mildly raised.