Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Necrotising Enterocolitis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
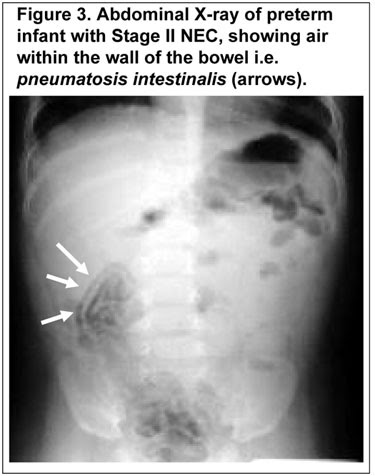
⚠️ Necrotising Enterocolitis (NEC) affects ~5% of infants with birth weights <1,500g. It often presents with abdominal distension, bloody stools, bile-stained vomiting, and the classic radiological finding of pneumatosis intestinalis.
🍼 About
- NEC is a life-threatening gastrointestinal emergency, almost exclusively affecting premature neonates.
- It can lead to bowel perforation, peritonitis, septic shock, and death.
- Mortality remains high (20–30%), especially with advanced disease.
⚡ Aetiology & Pathophysiology
- Immature intestinal mucosa + impaired barrier function.
- Combination of ischaemia–reperfusion injury, bacterial invasion, and an exaggerated inflammatory response.
- Inflammatory mediators (PAF, TNF, cytokines) → necrosis of intestinal wall.
📌 Risk Factors
- Prematurity & very low birth weight (VLBW).
- Formula feeding ❌ (breastfeeding protective).
- Congenital heart disease (↓ mesenteric perfusion).
- Polycythaemia, PDA, or use of umbilical arterial catheters near mesenteric arteries.
- Medications: Indomethacin, steroids (with indomethacin).
- Maternal factors: Cocaine exposure, perinatal hypoxia.
🩺 Clinical Presentation
- Feeding intolerance or bilious vomiting 💚.
- Abdominal distension, tenderness, wall oedema, or palpable mass.
- Blood-stained stools 💩.
- Absent bowel sounds, shock, apnoea, bradycardia in severe disease.
- Signs of perforation → rigid abdomen, peritonitis, rapid collapse.
🔬 Investigations
- Bloods: ↑ WCC/CRP, ↑ lactate, thrombocytopenia, coagulopathy (DIC).
- U&E: AKI, hyponatraemia.
- Blood gas: Metabolic acidosis (classic).
- AXR: Pneumatosis intestinalis (gas in bowel wall), portal venous gas, free air (if perforation).
📊 Staging – Bell’s Criteria
| Stage | Clinical Features | Investigations |
|---|---|---|
| Stage I (Suspected) | Feeding intolerance, abdominal distension, occult/visible blood in stool, apnoea, bradycardia | AXR: non-specific, mild distension |
| Stage II (Definite) | Absent bowel sounds, tenderness, systemic illness | Pneumatosis intestinalis or portal venous gas, metabolic acidosis, thrombocytopenia |
| Stage III (Advanced) | Severe illness, peritonitis, shock, DIC | Pneumoperitoneum = perforation |
🛠️ Management
- Resuscitation: ABC, fluids, correct acidosis, oxygen/ventilation if needed. Morphine for pain.
- Medical (first-line in suspected/early cases):
- Nil by mouth (NBM) 🚫🍼
- IV fluids & TPN
- Broad-spectrum IV antibiotics
- NG tube for decompression
- Surgical:
- Consult urgently if pneumoperitoneum, peritonitis, or clinical deterioration.
- Options: bowel resection ± stoma, or peritoneal drain in VLBW infants.
- Special situations: Avoid indomethacin in PDA with NEC. Consider PDA closure surgically.
⚠️ Complications
- Sepsis & peritonitis → multiorgan failure.
- Intestinal strictures (esp. colon).
- Short bowel syndrome → prolonged TPN dependence.
📚 References
Cases — Necrotising Enterocolitis (NEC) 👶🩺
- Case 1 — Preterm Baby with Distended Abdomen 🌡️: A 28-week preterm infant, day 10 of life, develops abdominal distension, bilious gastric aspirates, and bloody stools. Exam: tender abdomen, reduced bowel sounds. Abdominal X-ray: pneumatosis intestinalis. Diagnosis: NEC in very preterm infant. Management: Stop enteral feeds (NPO), NG decompression, IV antibiotics, supportive fluids; surgical review if perforation.
- Case 2 — Term Baby with Congenital Heart Disease 💔: A 3-day-old term neonate with hypoplastic left heart syndrome develops abdominal distension and fresh blood per rectum after formula feeding. CXR: portal venous gas. Diagnosis: NEC in term infant, precipitated by poor gut perfusion (CHD). Management: Supportive (IV fluids, antibiotics, NPO), optimise cardiac status, surgical team involvement if perforation/peritonitis suspected.
- Case 3 — Complicated NEC with Perforation ⚠️: A 2-week-old preterm neonate suddenly deteriorates with apnoea, abdominal wall erythema, and shock. Abdominal X-ray: free intraperitoneal air. Diagnosis: NEC complicated by intestinal perforation and peritonitis. Management: Emergency surgical intervention (laparotomy ± resection), broad-spectrum antibiotics, intensive care support.
Teaching Commentary 🧠
NEC = acute intestinal necrosis, mainly in preterm neonates. - Risk factors: prematurity, formula feeding, hypoxic/ischaemic events, congenital heart disease. - Clinical features: feeding intolerance, abdominal distension, bloody stools, sepsis. - Key radiology: pneumatosis intestinalis (air in bowel wall), portal venous gas, free air (perforation). - Management: Stop feeds, NG decompression, broad-spectrum antibiotics, fluid resuscitation, surgical referral if perforation/necrosis. ⚠️ Mortality is high; survivors may develop short bowel syndrome or strictures.