Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Motor Neuron Disease (MND-ALS)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Neurological History taking |Motor Neuron Disease (MND-ALS) |Miller-Fisher syndrome |Guillain Barre Syndrome |Multifocal Motor Neuropathy with Conduction block |Multiple Sclerosis (MS) Demyelination |Inclusion Body Myositis |Cervical spondylosis |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome |Spinal Cord Compression |Spinal Cord Haematoma |Spinal Cord Infarction
🧠 Motor Neurone Disease (MND) presents with generalized and bulbar weakness, muscle wasting, brisk reflexes, and no sensory loss. Eye and bladder function are typically spared. ⚡ There is no definitive diagnostic test — diagnosis relies on clinical signs involving both the brain and spinal cord.
About
- Also known as Amyotrophic Lateral Sclerosis (ALS), Charcot's disease, and Lou Gehrig's disease.
- ⏳ Diagnosis is often delayed, sometimes taking >16 months from symptom onset.
- Initial symptoms may be vague, e.g., fatigue or weakness.
How Common Is It? 📊
- Incidence: 1.8–2.2 per 100,000 population.
- Prevalence: 4.0–4.7 per 100,000 population in the UK.
- At any given time, ~2,000 individuals in England and Wales are affected.
Pathology 🔬
- Degeneration of motor giant pyramidal Betz cells (layer V, primary motor cortex).
- Loss of anterior horn cells in the spinal cord.
- Degeneration of cranial motor nuclei in the brainstem.
Aetiology / Genetics 🧬
- 🌍 Guam variant: linked with dementia & parkinsonism in the Chamorro people.
- SOD1 mutations implicated in familial ALS.
- Other mutations: RNA processing, axonal transport, cytoskeletal proteins.
- Familial ALS = ~10% of cases, usually autosomal dominant.
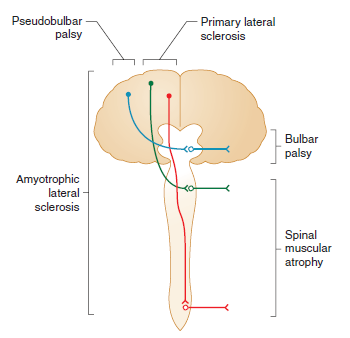
Forms of MND 🧾
- Progressive Muscular Atrophy: LMN predominant. ⏳ Survival 5–10 yrs.
- Progressive Bulbar Palsy: Tongue wasting, fasciculations, spastic palate. ⏳ Survival 2–3 yrs.
- Primary Lateral Sclerosis: UMN predominant, symmetrical. 👍 Good prognosis.
- ALS: UMN + LMN features. ⏳ Survival 3–4 yrs.
- MND-Dementia: Associated with FTD (frontotemporal dementia).
Clinical Features ⚠️
- 💪 Subtle weakness → progresses to wasting & fasciculations (esp. hands).
- 🌙 Painful nocturnal cramps (thighs common).
- Mixed UMN + LMN signs: weakness + brisk reflexes + extensor plantar.
- 🙅♂️ No significant sensory loss; eye movements & sphincters spared.
- 👅 Bulbar involvement: wasted fibrillating tongue, dysarthria, dysphagia.
- ⚖️ Weight loss due to dysphagia & wasting.
- “Dropped head” & wasted hands appearance.
El Escorial Criteria 📋
- Clinically Definite ALS: UMN + LMN signs in ≥3 regions (bulbar, cervical, thoracic, lumbar).
- Clinically Probable ALS: UMN + LMN in 2 regions, UMN above LMN.
- Clinically Possible ALS: UMN + LMN in 1 region only.
Differential Diagnosis 🔍
- MMN with conduction block (check GM-1 antibodies).
- Cervical spondylotic myelopathy, foramen magnum lesions (MRI).
- CIDP, Inclusion Body Myositis.
- Myasthenia Gravis (Tensilon, antibodies, EMG).
- Kennedy’s syndrome (X-linked).
- B12 deficiency, Lyme disease, malignancy.
Investigations 🧪
- FBC, U&E, TFT, CK, syphilis serology.
- CSF: may show mild ↑ protein.
- Autoantibody panel (exclude mimics).
- MRI brain/cervical spine → rule out mimics (syrinx, compression, vascular).
- EMG: fasciculations + fibrillation (LMN loss).
- Nerve conduction: often normal until late.
Management 🩺
- 👩⚕️ Multidisciplinary Support: Physio, OT, SALT, dietician, palliative input.
- 💊 Riluzole 50mg bd: Glutamate antagonist → extends survival by ~2–3 months.
- 💧 Anticholinergics: Glycopyrrolate, amitriptyline, or hyoscine for drooling.
- 🦵 Baclofen / Diazepam: Spasticity control.
- 🥤 Feeding support: NG, PEG, or RIG feeding when bulbar involvement advances.
- 😴 NIV (BiPAP): Improves sleep, reduces fatigue, ↑ survival by ~6 months.
- 🗣️ Speech synthesizers: Assist communication.
- 💊 Quinine, Carbamazepine, Gabapentin → muscle cramps.
- 🙂 SSRIs or mood stabilisers for depression & emotional lability.
Prognosis 📉
- Median survival: 2–3 yrs from diagnosis.
- ~25% survive ≥5 yrs.
References 📚
Cases — Motor Neurone Disease (MND)
- Case 1 — Amyotrophic Lateral Sclerosis (ALS, Mixed UMN & LMN) ⚡: A 58-year-old man presents with progressive weakness in his right hand, muscle fasciculations, and stiffness in his legs. Exam: wasting of hand intrinsic muscles, brisk reflexes, extensor plantar responses. No sensory loss. Diagnosis: ALS (most common form of MND). Management: Riluzole to modestly extend survival; physiotherapy; MDT input; NIV (non-invasive ventilation) for respiratory support.
- Case 2 — Progressive Bulbar Palsy 🗣️: A 62-year-old woman presents with slurred speech, difficulty swallowing, and choking on liquids. Exam: tongue wasting with fasciculations, brisk jaw jerk, nasal dysarthria. Diagnosis: Bulbar-onset MND (progressive bulbar palsy). Management: MDT care; speech and language therapy; gastrostomy for nutrition; NIV; symptomatic treatment of sialorrhoea.
- Case 3 — Primary Lateral Sclerosis (PLS, UMN-Predominant) 🧠: A 50-year-old man presents with progressive leg stiffness and spastic gait over 3 years. Exam: pyramidal weakness, brisk reflexes, extensor plantar responses, but no fasciculations or wasting. Sensation intact. Diagnosis: Primary lateral sclerosis (UMN-predominant MND variant). Management: Supportive — physiotherapy, spasticity control (baclofen, tizanidine), MDT monitoring.
Teaching Commentary 🧠
MND is a group of progressive neurodegenerative disorders of upper and lower motor neurones. - ALS: UMN + LMN signs, most common. - Bulbar Palsy: speech and swallowing first; poorer prognosis. - PLS: UMN-predominant; slower progression. - PMA (progressive muscular atrophy): LMN-predominant. Clues: weakness with fasciculations, mixed UMN/LMN signs, no sensory loss, progressive. Dx: clinical + EMG (denervation); MRI excludes mimics. Mx: Riluzole, multidisciplinary care, NIV, gastrostomy, palliative support. Prognosis: average survival 2–5 years (longer in PLS).