Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Arrhythmogenic Right Ventricular Cardiomyopathy
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Ventricular Tachycardia |Right Ventricular Outflow Tract Tachycardia |Resuscitation - Adult Tachycardia Algorithm |Automatic Implantable Cardioverter Defibrillator (AICD)
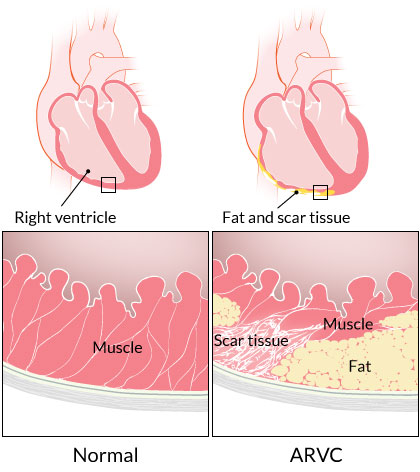
⚡ ARVC is part of the group of arrhythmogenic cardiomyopathies, characterised by fibrofatty replacement of the myocardium, most commonly the right ventricle. It carries a major risk of sudden cardiac death (SCD) due to malignant ventricular arrhythmias, particularly during exertion. 📌 Early recognition and consideration of ICD implantation is essential.
📖 About
- Also known as Arrhythmogenic Right Ventricular Dysplasia (ARVD).
- Initially affects the right ventricle, but studies show progressive left ventricular involvement over time → can become a biventricular disease.
- Prevalence: ~1 in 5,000–10,000 (likely underdiagnosed).
- Important cause of sudden cardiac arrest in young athletes. 🏃♂️⚠️
🧬 Genetics
- Usually autosomal dominant inheritance with variable penetrance.
- More than 8 implicated genes, mostly affecting desmosomal proteins (responsible for cell–cell adhesion in myocardium).
- Ask about family history of arrhythmia or sudden unexplained death.
- Accounts for up to 20% of sudden cardiac deaths in young people.
🧪 Key Genes
- Plakophilin-2 (PKP2)
- Desmoplakin (DSP)
- Desmoglein-2 (DSG2)
- Desmocollin-2 (DSC2)
- Plakoglobin (JUP)
- TMEM43
- RYR2 (linked to calcium handling abnormalities)
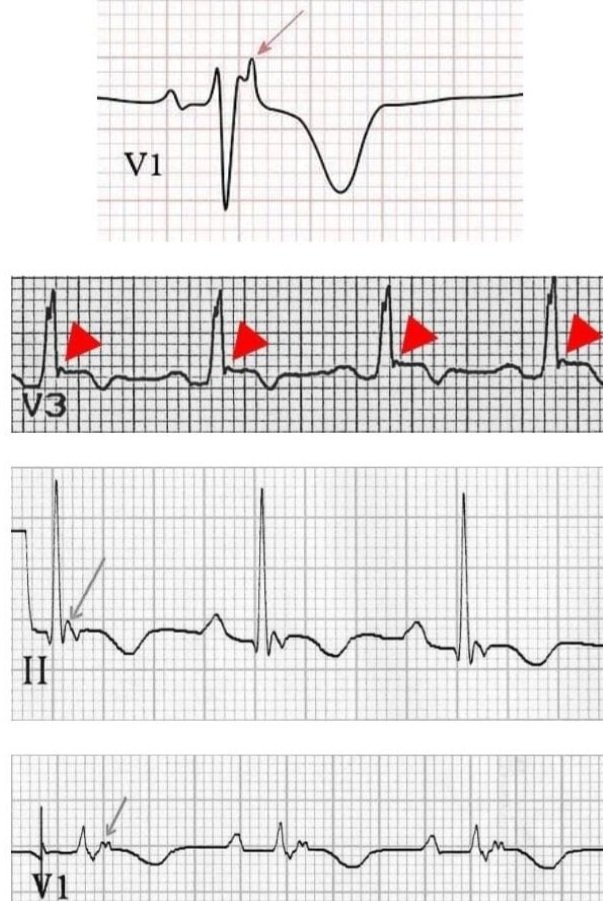
📸 ECG – Epsilon Waves
🩺 Aetiology / Pathology
- Mutations in desmosomal proteins weaken mechanical junctions → myocyte detachment & death → fibro-fatty replacement of myocardium.
- Predominantly affects RV free wall, outflow tract, and apex (“triangle of dysplasia”).
- Progressive thinning of RV wall → aneurysm formation → arrhythmia substrate.
- Subtypes: RV-dominant, biventricular, and LV-dominant ARVC.
🩺 Clinical Features
- Palpitations/fluttering (ectopics, atrial fibrillation, ventricular tachycardia).
- Exertional syncope or chest pain.
- Dyspnoea from RV failure in advanced disease.
- Dizziness, fatigue, abdominal discomfort from hepatomegaly / venous congestion.
- Exam: Widely split S2, S3 or S4 gallop; later signs of right heart failure.
⚠️ Complications
- Arrhythmias → ventricular ectopics, AF, VT, VF (leading cause of death).
- Progressive biventricular heart failure.
- Bradyarrhythmias, AV block.
- Sudden cardiac death, often during exertion.
🔍 Investigations
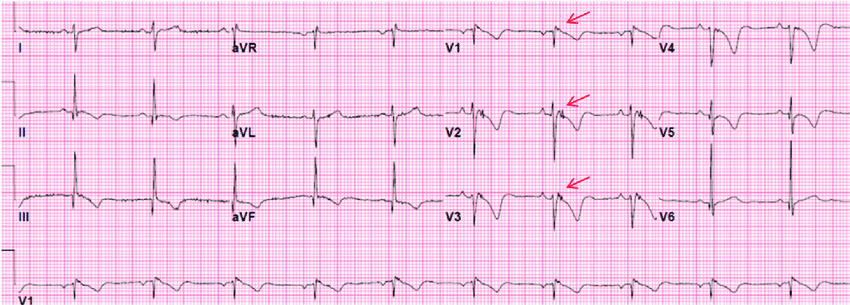
- ECG: T-wave inversion in V1–V3, epsilon waves (terminal notching), incomplete RBBB, VT with LBBB morphology.
- Echocardiogram: RV dilation, akinesis/dyskinesis, prominent trabeculations, RVOT dilatation.
- Cardiac MRI: gold standard → RV structural/functional abnormalities + tissue characterization (fibrofatty infiltration).
- Holter/monitoring: detect ventricular arrhythmias of RV or LV origin.
- Endomyocardial biopsy: rarely used, limited sensitivity due to patchy disease.
🔎 Differentials
- Idiopathic RV outflow tract tachycardia (benign, no fibrosis).
- Brugada syndrome (channelopathy with similar arrhythmia risk).
- RV volume overload from congenital lesions (e.g., ASD, Ebstein anomaly).
📸 ECG Showing Epsilon Waves
👨👩👧 Screening
- All first-degree relatives: 12-lead ECG + cardiac imaging; consider signal-averaged ECG.
- Genetic testing if pathogenic variant identified in proband.
- Family follow-up essential as penetrance increases with age.
💊 Management
- Lifestyle: Avoid competitive or high-intensity sports, caffeine, stimulants. Moderate daily activity only.
- ICD: definitive therapy for high-risk or survivors of cardiac arrest / sustained VT.
- Antiarrhythmics: beta-blockers (mainstay), sotalol, amiodarone for VT suppression.
- Catheter ablation: option for recurrent VT refractory to drugs; often palliative (high recurrence).
- Heart failure therapy: ACEi/ARB, diuretics, MRA as indicated.
- Anticoagulation: if atrial fibrillation present.
- Transplantation: end-stage cases with refractory HF or arrhythmias.
- 🔁 Lifelong cardiology follow-up in specialist inherited cardiac conditions clinic.
📚 References
- 2019 HRS Consensus on Arrhythmogenic Cardiomyopathy
- CSANZ Guidelines – Diagnosis & Management of ARVC
Cases — Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
- Case 1 — Sudden Cardiac Symptoms in a Young Athlete: A 22-year-old semi-professional footballer collapses during training with palpitations and presyncope. ECG shows T-wave inversion in V1–V3 and episodes of ventricular tachycardia with left bundle branch block (LBBB) morphology. Echo and MRI demonstrate right ventricular dilation and regional wall motion abnormalities. Family history: cousin died suddenly at age 19. Diagnosis: ARVC presenting with exertional arrhythmia and risk of sudden cardiac death.
- Case 2 — Palpitations and Heart Failure in Middle Age: A 45-year-old man presents with progressive exertional dyspnoea, ankle swelling, and recurrent palpitations. ECG shows frequent ventricular ectopics. Cardiac MRI reveals fibro-fatty replacement of the right ventricular free wall with impaired systolic function. Genetic testing: plakophilin-2 mutation. Diagnosis: ARVC with arrhythmia and right-sided heart failure.
Teaching Commentary ❤️
ARVC is a rare inherited cardiomyopathy (often autosomal dominant, desmosomal gene mutations such as PKP2, DSG2, DSP) where fibro-fatty replacement of the right ventricular myocardium predisposes to ventricular arrhythmias, heart failure, and sudden cardiac death. Typical features: - Young adults, especially athletes. - ECG: T-wave inversion in V1–V3, epsilon waves, ventricular tachycardia with LBBB morphology. - Imaging: RV dilation/dyskinesia, fatty infiltration. Diagnosis uses the Task Force Criteria (structural, histological, ECG, arrhythmic, and family/genetic). Management: exercise restriction, implantable cardioverter-defibrillator (ICD) for sudden death prevention, anti-arrhythmics, and heart failure therapy if needed.