Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
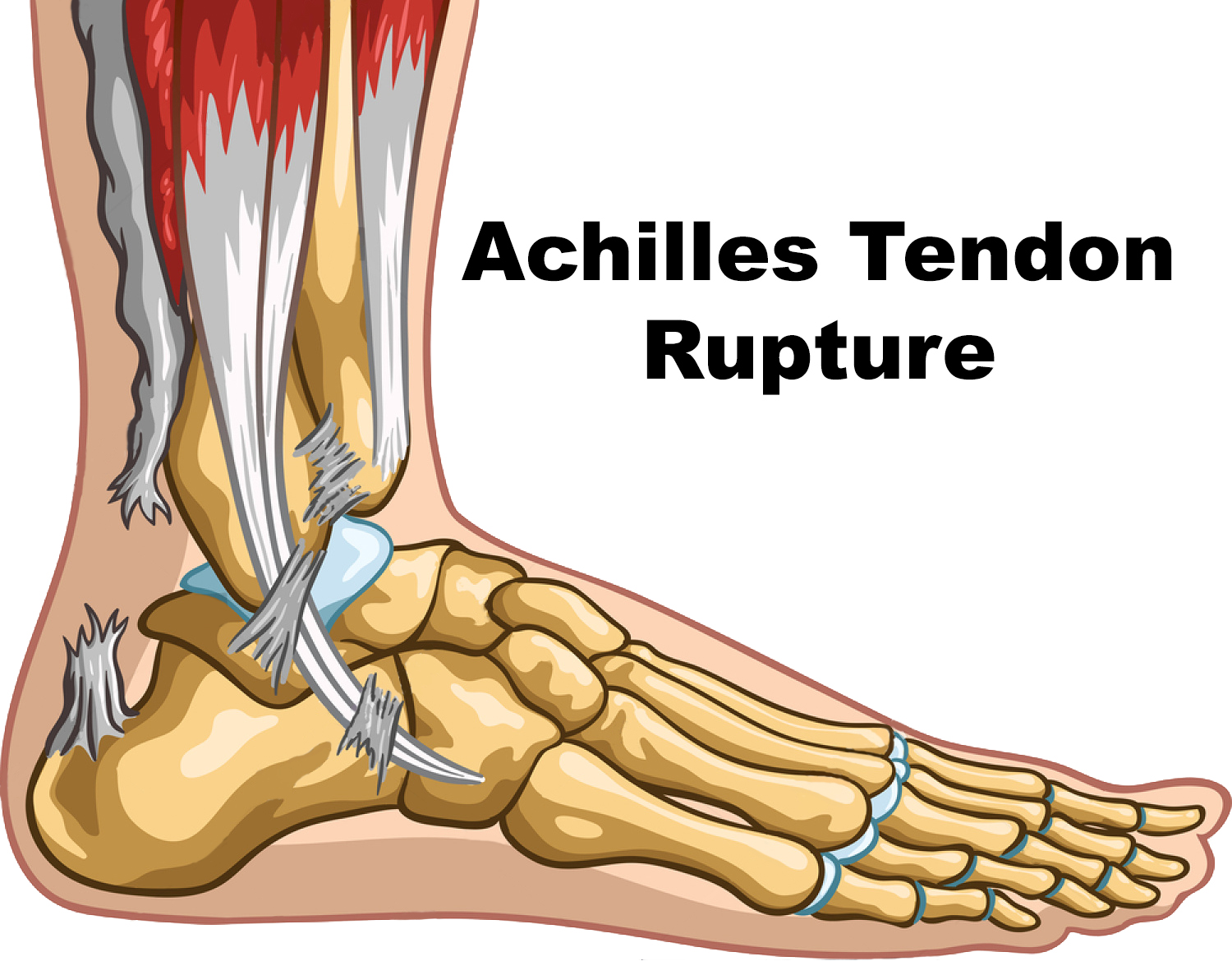
Achilles Tendon rupture
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🦶 Achilles tendon ruptures are classically described as a sudden "snap" or "kick" at the back of the ankle, often during sport. 🚫 Risk factors include fluoroquinolones, corticosteroid injections, diabetes, and increasing age. 🔎 The Thompson calf squeeze test is the hallmark diagnostic sign. ⚖️ Non-surgical treatment carries a higher re-rupture risk, while surgery reduces recurrence but increases wound complications.
📖 About Achilles Tendon Injury
- Despite being the strongest tendon in the body, the Achilles is prone to rupture under sudden eccentric load (jumping, sprinting).
- Often termed the “weekend warrior injury”, it typically affects middle-aged recreational athletes.
⚠️ Aetiology & Risk Factors
- Repetitive sporting stress or sudden acceleration/deceleration.
- Degenerative thinning with age, worsened by diabetes or arthritis.
- Medication-related: fluoroquinolones (e.g. ciprofloxacin), repeated corticosteroid injections.
- Other: obesity, poor conditioning, and systemic inflammatory disease.
🩺 Clinical Features
- Sudden sharp "snap" or "kick" sensation in the heel/ankle, sometimes audible.
- Weakness in plantarflexion; patients may walk flat-footed but cannot run or stand on tiptoe on the injured side.
- Palpable gap along tendon course.
- Thompson test: calf squeeze fails to cause plantar flexion (positive test).
- Partial ruptures: more subtle, may still allow limited tiptoe standing with both feet.
🔍 Investigations
- Ultrasound: First-line, dynamic, identifies site and extent of rupture.
- MRI: Reserved for equivocal cases or surgical planning.
💊 Management
- Non-surgical: Rest, ice, compression, elevation (RICE), functional bracing/boot in plantarflexion; suitable for partial tears or less active patients.
- Surgical repair: End-to-end tendon suturing; preferred in complete tears and active individuals. Allows faster rehab but carries wound/DVT risk.
- Rehabilitation: Physiotherapy essential for both strategies. Gradual strengthening, stretching, and proprioception training. Return to sport may take 6–12 months.
⚡ Complications
- Re-rupture (higher with conservative treatment).
- Wound healing problems, infection, adhesions (surgery).
- Chronic calf weakness or muscle atrophy.
- DVT risk with immobilisation.
🩺 Case 1 — Sudden Sports Injury
A 34-year-old man felt a sudden "pop" in the back of his ankle while playing football, followed by severe pain and difficulty walking. On exam: swelling over the Achilles tendon, positive Thompson’s test (no plantarflexion on calf squeeze), and inability to stand on tiptoe. Management: 🏥 Immobilisation in plantarflexion (cast or functional brace), early orthopaedic referral. Surgical repair often offered to young/active patients. Physiotherapy essential for rehab. Avoid: ❌ Missing the diagnosis by assuming it is a simple ankle sprain; avoid weight-bearing until stabilised.
🩺 Case 2 — Older Patient on Steroids
A 65-year-old man on long-term prednisolone for COPD presents with sudden pain and weakness in the left ankle after stepping off a curb. Exam: palpable gap in the Achilles tendon, weak plantarflexion, and difficulty walking. Management: 💊 Non-surgical management with functional bracing may be appropriate given comorbidities; analgesia and physiotherapy. Surgical repair if fit and active. Avoid: ❌ Continuing steroids or fluoroquinolones without review (increase rupture risk); avoid prolonged immobilisation without venous thromboembolism prophylaxis.