Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Red Blood Cells
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Red blood cells |White blood cells |Lymphocytes |Platelets |Cryoprecipitate |Fresh Frozen Plasma |d Blood Cell Maturation
Overview of Erythrocytes / Red Blood Cells
Erythrocytes, also known as red blood cells (RBCs), are the most abundant cell type in the blood and are essential for transporting oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs for exhalation. RBCs are uniquely adapted to perform this critical function through their specialized structure and composition.
Structure of Red Blood Cells
- RBCs have a biconcave disc shape:
- Increases surface area for gas exchange.
- Provides flexibility to navigate through narrow capillaries.
- Mature RBCs lack a nucleus and organelles:
- Maximizes space for haemoglobin, the oxygen-carrying protein.
- Prevents consumption of the oxygen they transport.
- Haemoglobin (Hb) is the main component:
- Composed of four globin chains, each with a heme group that binds oxygen.
- Each haemoglobin molecule can carry four oxygen molecules.
Function of Red Blood Cells
- Oxygen Transport :
- RBCs pick up oxygen in the lungs where it binds to haemoglobin.
- Transport oxygen to tissues where it is released for cellular respiration.
- Carbon Dioxide Transport :
- RBCs collect carbon dioxide, a waste product of metabolism, from tissues.
- Transport it to the lungs where it is expelled from the body.
- CO₂ is transported in three forms: dissolved in plasma, as bicarbonate ions (HCO3-), and bound to haemoglobin (carbaminohaemoglobin).
- Buffering Blood pH :
- Haemoglobin acts as a buffer by binding hydrogen ions (H+), helping to maintain acid-base balance in the blood.
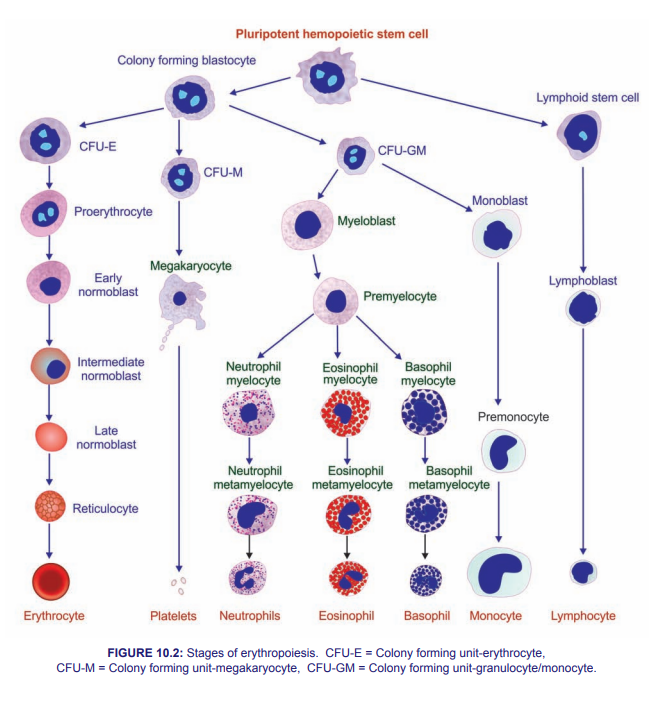
Erythropoiesis
- Erythropoiesis is the process of red blood cell production:
- Occurs in the bone marrow.
- Stimulated by erythropoietin (EPO), a hormone produced by the kidneys in response to hypoxia (low oxygen levels).
- Stages of development include:
- Hematopoietic stem cells differentiate into erythroid progenitor cells.
- Progenitor cells become proerythroblasts, then erythroblasts, which synthesize haemoglobin.
- Reticulocytes (immature RBCs) are released into the bloodstream and mature into erythrocytes within a few days.
Life Cycle of Red Blood Cells
- RBCs have a lifespan of approximately 120 days.
- Aging RBCs are removed from circulation by macrophages in the spleen, liver, and bone marrow.
- Haemoglobin is broken down:
- Globin proteins are degraded into amino acids.
- Heme is split into iron, which is recycled, and biliverdin, which is converted to bilirubin and excreted in bile.
Clinical Relevance
- Anaemias :
- Conditions characterized by a decrease in the number or function of RBCs, leading to reduced oxygen-carrying capacity.
- Causes include nutritional deficiencies (iron, vitamin B12, folate), genetic disorders (sickle cell anaemia, thalassemias), and chronic diseases.
- Symptoms include fatigue, pallor, shortness of breath, and dizziness.
- Polycythaemia :
- A condition characterized by an increased number of RBCs, which can lead to increased blood viscosity and risk of thrombosis.
- Can be primary (due to bone marrow disorders) or secondary (due to chronic hypoxia or tumours producing EPO).
- Haemolytic Disorders :
- Conditions where RBCs are destroyed faster than they can be produced.
- Causes include autoimmune diseases, infections, certain medications, and genetic conditions (e.g., G6PD deficiency).
Summary
Red blood cells are crucial for transporting oxygen and carbon dioxide, as well as maintaining acid-base balance in the blood. Their unique structure and composition enable them to perform these functions efficiently. Understanding erythropoiesis, the life cycle of RBCs, and related clinical conditions is essential for diagnosing and treating various hematological disorders.
Overview of the Red Cell Membrane
The red cell membrane is a complex structure that provides erythrocytes (red blood cells) with the flexibility and durability needed to survive in the circulatory system. It plays crucial roles in maintaining cell shape, enabling deformability, and ensuring the proper function of red blood cells.
Structure of the Red Cell Membrane
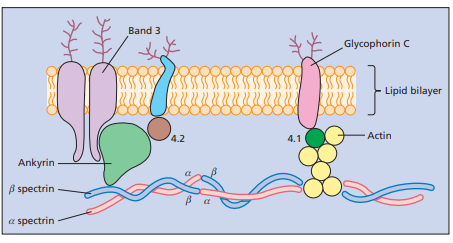
- The red cell membrane is composed of a lipid bilayer, membrane proteins, and an underlying cytoskeletal network:
- Lipid Bilayer :
- Composed of phospholipids, cholesterol, and glycolipids.
- Provides a semi-permeable barrier, allowing selective transport of ions and molecules.
- Phospholipids are arranged with hydrophilic heads facing outward and hydrophobic tails inward.
- Membrane Proteins :
- Integral proteins span the lipid bilayer, while peripheral proteins are attached to the inner or outer surface.
- Key integral proteins include:
- Band 3: Anion exchanger that facilitates the transport of chloride and bicarbonate.
- Glycophorin: Provides negative charge to the cell surface, preventing aggregation.
- Peripheral proteins interact with the cytoskeleton and include:
- Spectrin: A key structural protein that forms a mesh-like network beneath the membrane.
- Actin: Works with spectrin to maintain cell shape and flexibility.
- Ankyrin: Anchors the spectrin-actin cytoskeleton to the lipid bilayer via Band 3.
- Cytoskeletal Network :
- Consists primarily of spectrin, actin, and associated proteins.
- Provides mechanical support and stability to the membrane.
- Allows the red blood cell to deform and squeeze through narrow capillaries.
- Lipid Bilayer :
Functions of the Red Cell Membrane
- Maintaining Cell Shape and Integrity :
- The membrane's structure ensures the biconcave shape of red blood cells, optimizing gas exchange.
- Provides mechanical strength to withstand the shear forces in circulation.
- Deformability :
- Enables red blood cells to change shape and pass through narrow capillaries and splenic sinusoids without rupturing.
- Flexibility is primarily due to the spectrin-actin cytoskeleton and its connections to the lipid bilayer.
- Selective Permeability :
- Controls the movement of ions and molecules into and out of the cell, maintaining osmotic balance and cell volume.
- Integral proteins such as ion channels and transporters facilitate this selective transport.
- Protection :
- The membrane's negative charge, provided by sialic acid residues on glycophorins, prevents red blood cells from clumping together.
- Protects the cell from mechanical damage and pathogen invasion.
- Cell Signaling :
- Membrane proteins are involved in cell signaling pathways that regulate red blood cell function and survival.
Clinical Relevance
- Hereditary Spherocytosis :
- Genetic disorder caused by defects in membrane proteins (e.g., spectrin, ankyrin).
- Leads to spherical-shaped red blood cells that are less flexible and more prone to haemolysis.
- Symptoms include anaemia, jaundice, and splenomegaly.
- Hereditary Elliptocytosis :
- Genetic disorder caused by mutations in genes encoding spectrin or other cytoskeletal proteins.
- Results in elliptical-shaped red blood cells with decreased deformability.
- May lead to haemolytic anaemia in severe cases.
- Paroxysmal Nocturnal Haemoglobinuria (PNH) :
- Acquired disorder resulting from mutations in the PIGA gene, affecting the synthesis of GPI anchors.
- Leads to a deficiency of GPI-anchored proteins that protect red blood cells from complement-mediated lysis.
- Symptoms include haemolysis, haemoglobinuria, and increased risk of thrombosis.
- Autoimmune Haemolytic Anaemia (AIHA) :
- Condition where the immune system produces antibodies that target red blood cell membrane proteins.
- Leads to premature destruction of red blood cells by the spleen and liver.
- Symptoms include fatigue, pallor, jaundice, and splenomegaly.
Summary
The red cell membrane is a dynamic and complex structure that ensures the proper function, shape, and survival of red blood cells. It consists of a lipid bilayer, integral and peripheral proteins, and a cytoskeletal network that provides mechanical support and flexibility. Understanding the structure and function of the red cell membrane is crucial for diagnosing and managing various hematological disorders.