Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Progressive Multifocal Leukoencephalopathy (PML)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Neurological History taking |Motor Neuron Disease (MND-ALS) |Miller-Fisher syndrome |Guillain Barre Syndrome |Multifocal Motor Neuropathy with Conduction block |Multiple Sclerosis (MS) Demyelination |Transverse myelitis |Acute Disseminated Encephalomyelitis |Progressive Multifocal Leukoencephalopathy (PML) |Inclusion Body Myositis |Cervical spondylosis |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome |Spinal Cord Compression |Spinal Cord Haematoma |Spinal Cord Infarction
🧠 Progressive Multifocal Leukoencephalopathy (PML) is a rare but devastating JC virus encephalopathy seen in immunocompromised patients. ⚠️ Always consider it in patients who have received Natalizumab or Rituximab therapy.
🔎 Introduction
- PML is caused by reactivation of the JC Virus (a human polyomavirus).
- Commonly associated with AIDS, advanced cancers, bone marrow transplantation, and immunosuppressive drugs.
- JC virus infects oligodendrocytes → causes patchy CNS demyelination.
- Most people (40–90%) carry latent JC virus asymptomatically, but reactivation occurs in immunosuppression.
⚠️ Aetiology
- JC Virus infection targeting oligodendrocytes → progressive demyelination.
- Triggered by:
- Severe immunosuppression (e.g., HIV with CD4 < 200).
- Immunosuppressive therapies: monoclonal antibodies, chemotherapy, steroids.
💊 Drug-Associated Causes
- Natalizumab (anti-α4 integrin, MS & Crohn’s).
- Rituximab (anti-CD20, haematological malignancies, autoimmune disease).
- Fingolimod (MS, sphingosine-1P modulator).
- Dimethyl fumarate (MS immunomodulator).
- Efalizumab (anti-CD11a).
- TNF inhibitors (adalimumab, infliximab, etanercept).
- Ruxolitinib (JAK 1/2 inhibitor).
🩺 Clinical Features
- Highly variable, depends on white matter lesion sites:
- ⚡ Focal weakness or sensory loss
- 🎯 Ataxia, brainstem signs
- 🧩 Cognitive impairment, confusion
- 👀 Visual disturbances
- Seizures can occur
🔍 Differential Diagnoses
- Multiple Sclerosis
- Susac Syndrome
- Glioma / CNS lymphoma
- In AIDS patients:
- Toxoplasmosis
- CNS Lymphoma
- Cryptococcal meningitis
- HIV encephalopathy
- CMV or HSV infection
🧪 Investigations
- Bloods: FBC, U&E, CRP; HIV serology, syphilis screen.
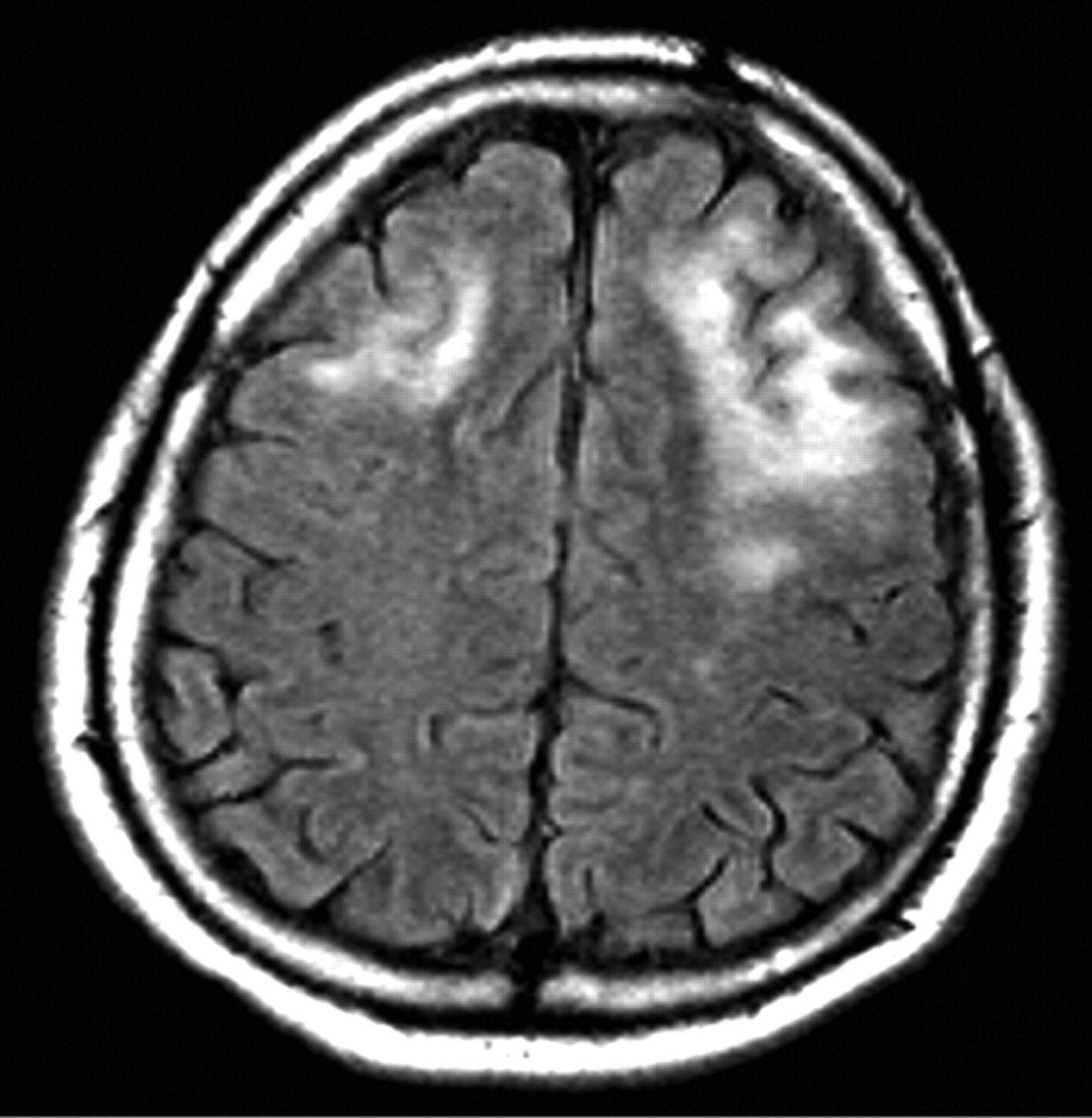
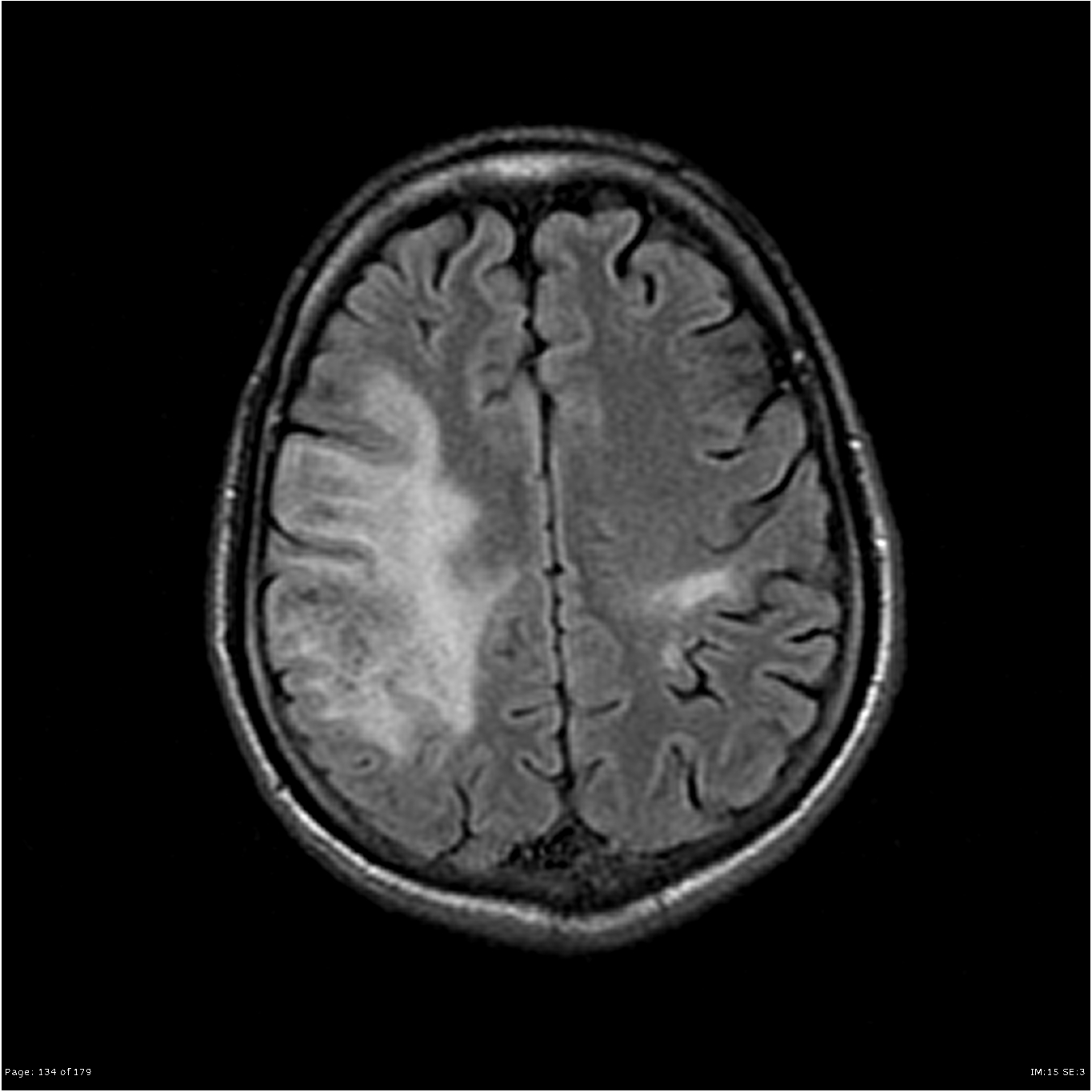
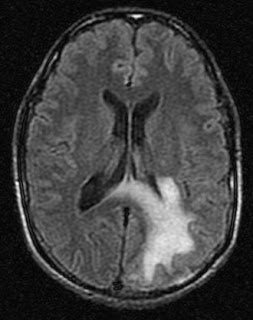
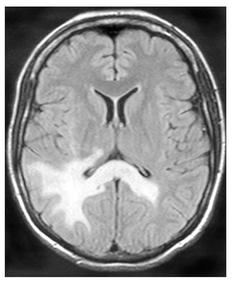
- MRI Brain: T2 hyperintense white matter lesions, often asymmetrical, involving parietal-occipital lobes, corpus callosum. May mimic MS or tumour.
- CSF: PCR for JC virus (diagnostic gold standard).
- Brain Biopsy: Rare but definitive when imaging/CSF inconclusive.
🖼️ Imaging
💊 Management
- HIV Patients: Start/optimise HAART → some recover if CD4 >200.
- IRIS (immune reconstitution inflammatory syndrome): Seen in 10–20% post-HAART, may worsen oedema. Steroids sometimes used.
- Drug-induced PML: Stop causative drug (e.g., Natalizumab, Rituximab).
- Antivirals / chemotherapy: Limited evidence for agents like Cidofovir or Cytarabine (ara-C).
- Supportive Care: Seizure control, neurorehab, ICP monitoring.
📉 Prognosis
- Without treatment: median survival ~6 months.
- With HAART: some long-term survival possible.
- Drug-associated PML: prognosis varies, depends on immune recovery after drug withdrawal.
📚 References
- Progressive Multifocal Leukoencephalopathy: New Concepts
- Clifford DB, et al. Neurology. 2010 – Natalizumab-associated PML risk factors.
- D'Souza A, et al. Lancet Neurology. 2019 – PML in immunotherapy.