Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Acute Promyelocytic Leukaemia (APML)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: | Leukaemias in General | Acute Promyelocytic Leukaemia | Acute Myeloblastic Leukaemia (AML) | Acute Lymphoblastic Leukaemia (ALL) | Chronic Lymphocytic Leukaemia (CLL) | Chronic Myeloid Leukaemia (CML) | Hairy Cell Leukaemia | Differentiation Syndrome | Tretinoin (All-trans-retinoic acid (ATRA)) | Haemolytic Anaemia | Immune (Idiopathic) Thrombocytopenic Purpura (ITP)
Acute Promyelocytic Leukaemia (APML) is a subtype of Acute Myeloid Leukaemia (AML) 🧬 characterized by the accumulation of abnormal promyelocytes in the bone marrow 🦴 and blood. It is distinct due to the translocation t(15;17), producing the PML-RARα fusion protein, which blocks normal differentiation of myeloid cells. APML carries a particularly high risk of Disseminated Intravascular Coagulation (DIC) ⚠️ but is also one of the most treatable forms of AML when identified promptly and treated with ATRA (all-trans-retinoic acid) and arsenic trioxide. ✨
About
- A rare AML subtype, accounting for ~10–15% of AML cases.
- Notable for its strong association with DIC at presentation and during treatment.
- ATRA therapy directly targets the differentiation block caused by PML-RARα, making APML highly curable compared to other AMLs. 🎯
🧪 Key teaching point: Always suspect APML if a patient presents with cytopenias, abnormal promyelocytes on film, and unexplained bleeding/DIC → start ATRA immediately, even before confirmation.
Aetiology
- Genetic driver: Reciprocal translocation t(15;17).
- PML gene (chr 15) fuses with RARα gene (chr 17) → PML-RARα protein.
- This fusion protein blocks myeloid cell maturation and promotes apoptosis resistance.
- Result: Accumulation of promyelocytes, marrow failure, coagulopathy, and infection risk.
Auer Rods in APML
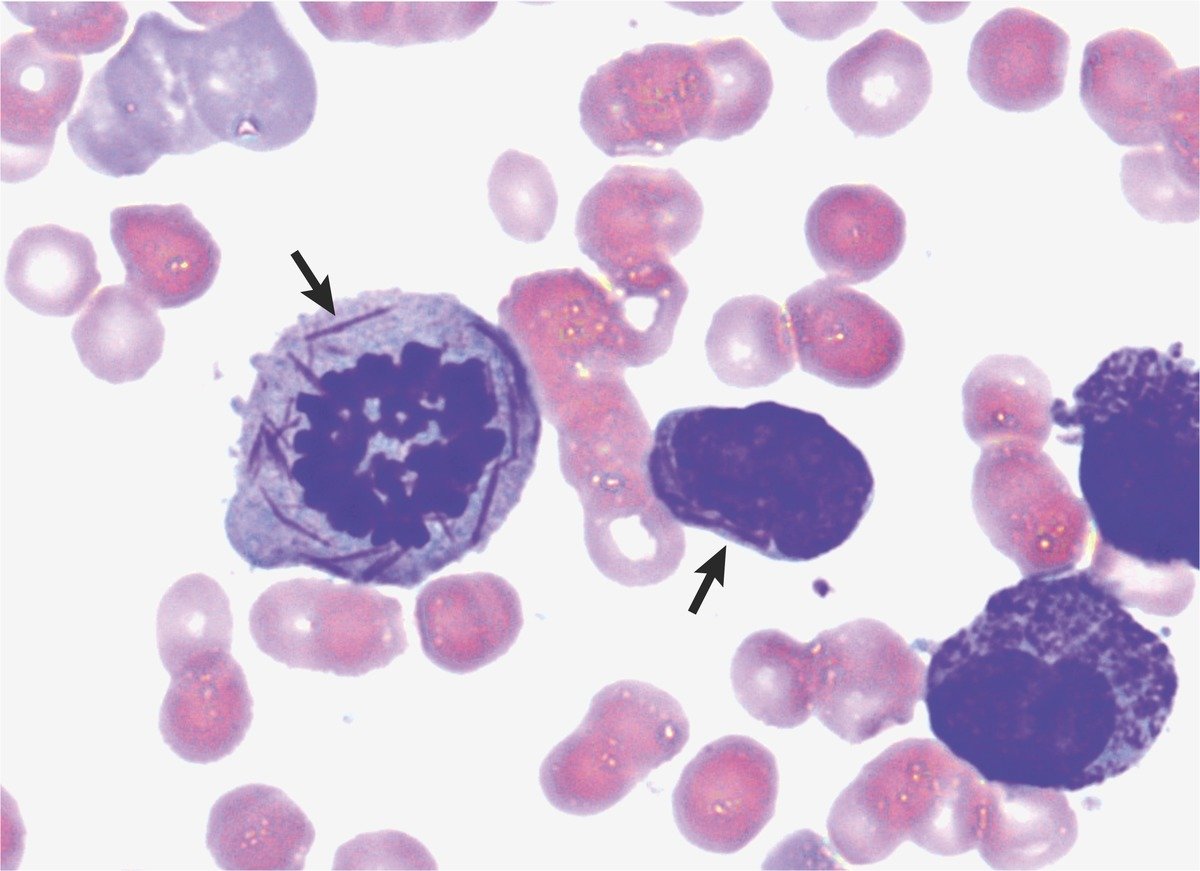
Auer rods (needle-like azurophilic inclusions) are often multiple and bundled (“faggot cells”) in APML 🔬
Clinical Features
- General AML symptoms: fatigue 😴, weight loss, anorexia.
- Marrow failure → anaemia, infections 🤒, bleeding 🩸.
- Bleeding risk disproportionately severe due to DIC (epistaxis, GI bleeding, intracranial haemorrhage).
- Low or high WCC possible, with abnormal promyelocytes visible on smear.
Investigations
- FBC: Pancytopenia with circulating promyelocytes.
- Coagulation screen: Prolonged PT/aPTT, low fibrinogen, raised D-dimer → DIC ⚠️
- Bone marrow biopsy: Abundant promyelocytes, often with “faggot” Auer rods.
- Cytogenetics: t(15;17) confirming diagnosis.
- Flow cytometry: Myeloid immunophenotype (CD33+, MPO+).
Management
- Urgent ATRA therapy: Vitamin A derivative that releases the differentiation block, allowing promyelocytes → mature neutrophils. ⭐
- Arsenic trioxide: Now standard with ATRA for front-line therapy; excellent remission rates.
- Anthracyclines (e.g. daunorubicin): Sometimes combined in high-risk disease.
- DIC management: Platelet transfusions (maintain >30–50 ×10⁹/L), FFP, cryoprecipitate for fibrinogen support.
- Tumour lysis prophylaxis: Hydration + allopurinol/rasburicase 💧
Differentiation Syndrome (formerly Retinoic Acid Syndrome)
- Occurs in up to 25% of patients within 3 weeks of ATRA initiation.
- Symptoms: Fever 🌡️, weight gain, dyspnoea, pulmonary infiltrates, pleural/pericardial effusions.
- Pathophysiology: Cytokine storm from rapidly differentiating myeloid cells.
- Management: High-dose IV dexamethasone 💊; temporary interruption of ATRA in severe cases.
Prognosis
- APML is now considered the most curable AML subtype 🎉
- Cure rates >85% with ATRA + arsenic-based regimens.
- Biggest danger = early death from haemorrhage (esp. intracranial) → emphasises need for immediate recognition and treatment.
References
🧑⚕️ Case Examples — Acute Promyelocytic Leukaemia (APML)
- Case 1 (Bleeding & DIC at presentation): ⚠️ A 29-year-old woman presents with gum bleeding, epistaxis, and widespread petechiae. Bloods: Hb 8.5 g/dL, WCC 3.0 × 10⁹/L, platelets 18 × 10⁹/L. Coagulation: prolonged PT, low fibrinogen, raised D-dimer. Blood film shows abnormal promyelocytes with Auer rods. Diagnosis: APML complicated by disseminated intravascular coagulation (DIC). Management: Start all-trans retinoic acid (ATRA) immediately (before cytogenetic confirmation), aggressive clotting factor replacement (cryoprecipitate, platelets, FFP), and urgent haematology referral.
- Case 2 (Incidental cytopenias): 🩸 A 42-year-old man referred by GP for unexplained bruising and fatigue. FBC shows Hb 9.1 g/dL, WCC 2.5 × 10⁹/L, platelets 30 × 10⁹/L. Coagulation screen shows early derangement. Peripheral smear: promyelocytes with heavy granules. Cytogenetics: t(15;17) translocation (PML-RARA fusion). Diagnosis: Acute Promyelocytic Leukaemia. Management: Immediate ATRA + arsenic trioxide initiated, with supportive transfusion strategy. Patient placed on tumour lysis prophylaxis (rasburicase, IV fluids). Prognosis good with rapid treatment.
- Case 3 (High WCC hyperleukocytosis): 🫁 A 36-year-old woman presents with dyspnoea, headache, and blurred vision. Bloods: WCC 85 × 10⁹/L, blasts with promyelocyte morphology, abnormal coagulation. Diagnosis: APML with hyperleukocytosis and risk of leukostasis. Management: Start ATRA immediately, plus induction chemotherapy (idarubicin + arsenic trioxide). ICU support for TLS risk, hydroxycarbamide to reduce leukocyte count. Close monitoring for differentiation syndrome once therapy initiated (managed with steroids if develops).