Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Abducent Nerve (Cranial Nerve VI)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Olfactory Nerve
|Optic Nerve
|Oculomotor Nerve
|Trochlear Nerve
|Trigeminal Nerve
|Abducent Nerve
|Facial Nerve
|Vestibulocochlear Nerve
|Glossopharyngeal Nerve
|Vagus Nerve
|Accessory Nerve
|Hypoglossal Nerve
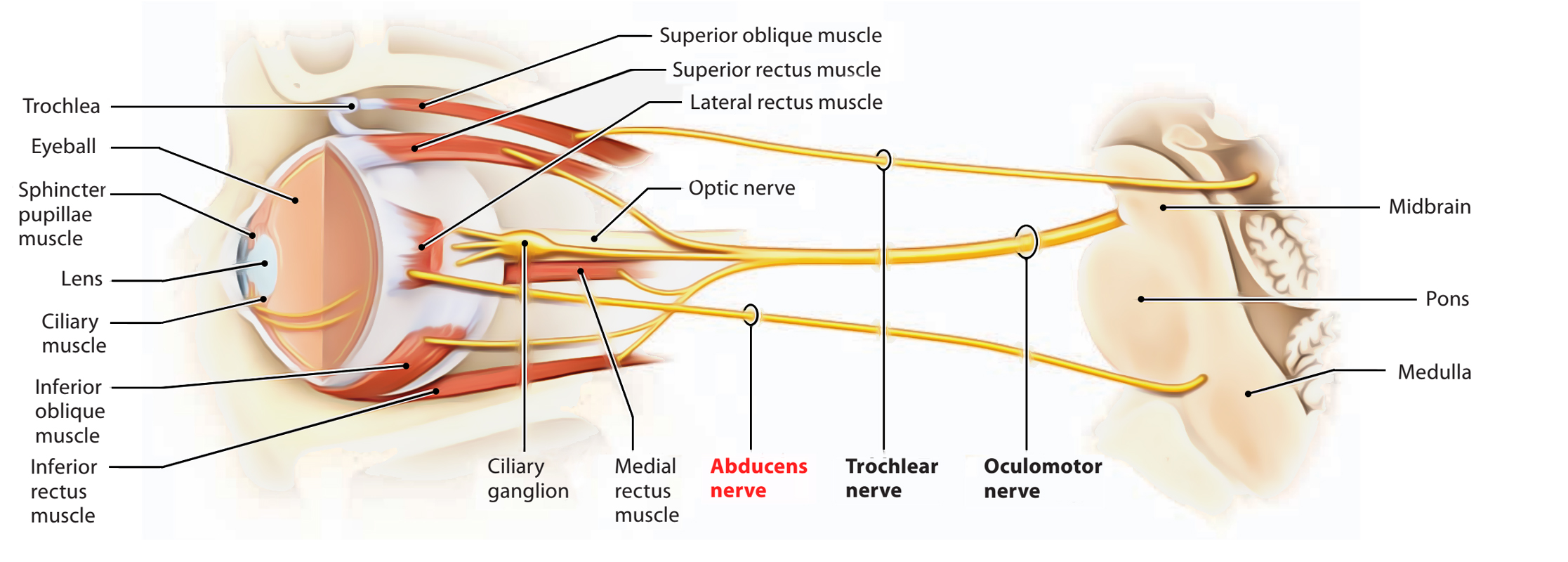
An ipsilateral VIIth nerve palsy alongside a VIth nerve palsy localises the lesion to the pons (facial colliculus).The abducent nerve (cranial nerve VI) is a pure motor nerve. It supplies the lateral rectus muscle, enabling abduction of the eye.
Anatomy
Function
Clinical Presentation
Common Causes
Cause Mechanism
Raised ICP Downward pressure stretches CN VI along clivus (most common isolated CN palsy in ICP).
Brainstem stroke (pons) Vascular infarct affecting VI nucleus/fascicle (basilar artery branches).
Tumour/compression Skull base tumours, nasopharyngeal carcinoma, meningioma.
Demyelination MS plaques in pons.
Diabetes Microvascular ischaemic mononeuropathy.
Trauma Fracture at skull base; direct nerve injury.
Myasthenia gravis Can mimic CN VI palsy (fatigable weakness).
Investigations
Management
References