Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Anatomy of the Stomach
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Anatomy of the Oesophagus |Anatomy of the Diaphragm |Anatomy of Large Bowel |Anatomy of Small Bowel |Anatomy of the Biliary system |Anatomy of the Eye |Anatomy of the Larynx |Anatomy of the Ear |Anatomy of the Pharynx |Anatomy of the Nose |Anatomy of Male Genitalia |Anatomy of Breast |Anatomy of the Stomach |Anatomy of the Rectum |Anatomy of the Spleen
Anatomy of the Stomach
-
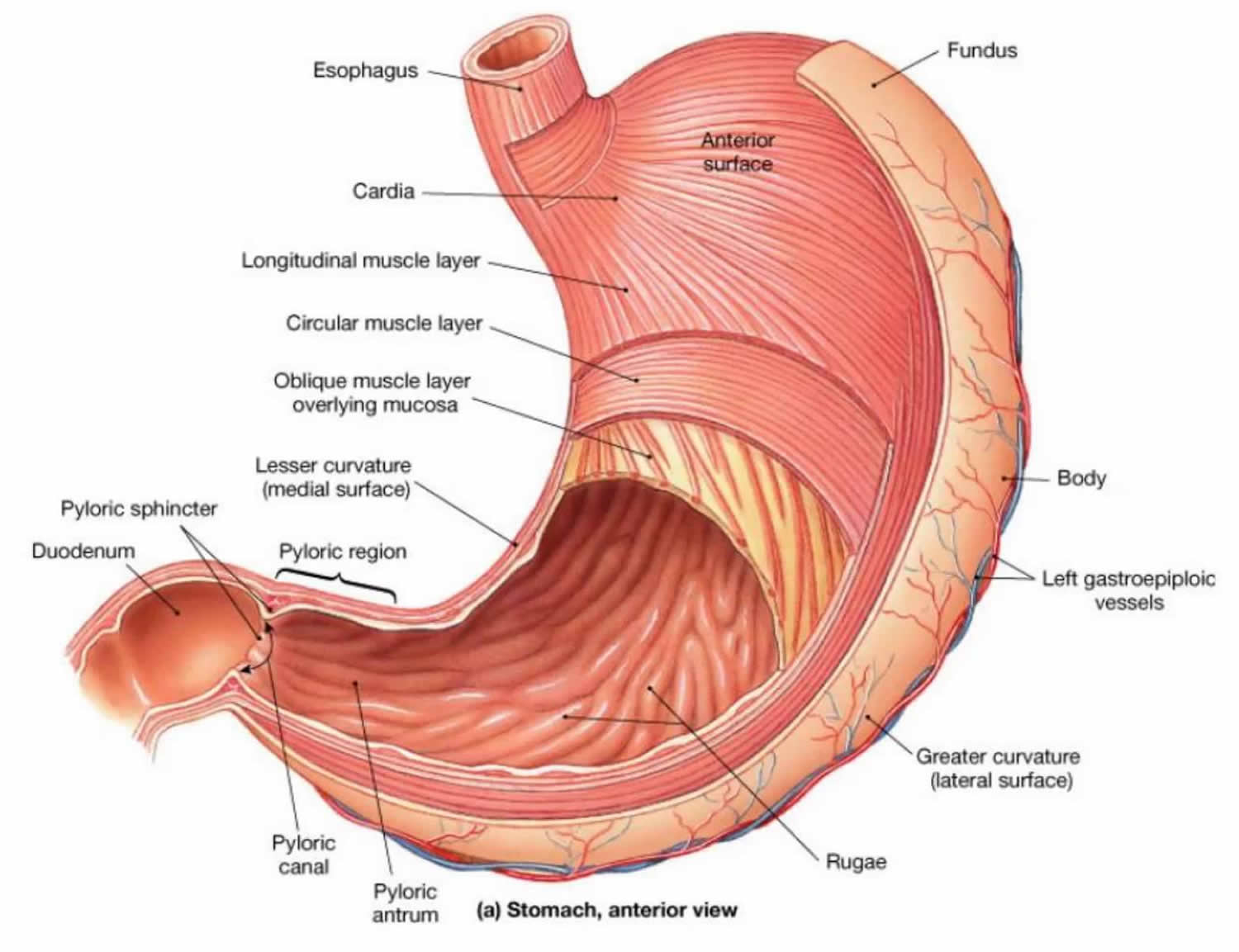
Regions of the Stomach:
- Cardia: The entry region where the oesophagus meets the stomach, guarded by the lower oesophageal sphincter.
- Fundus: The dome-shaped upper area, often containing air.
- Body: The central region where most digestion occurs.
- Antrum: The lower portion that grinds and mixes food into chyme.
- Pylorus: The exit region leading to the duodenum, containing the pyloric sphincter to regulate chyme passage.
-
Layers of the Stomach Wall:
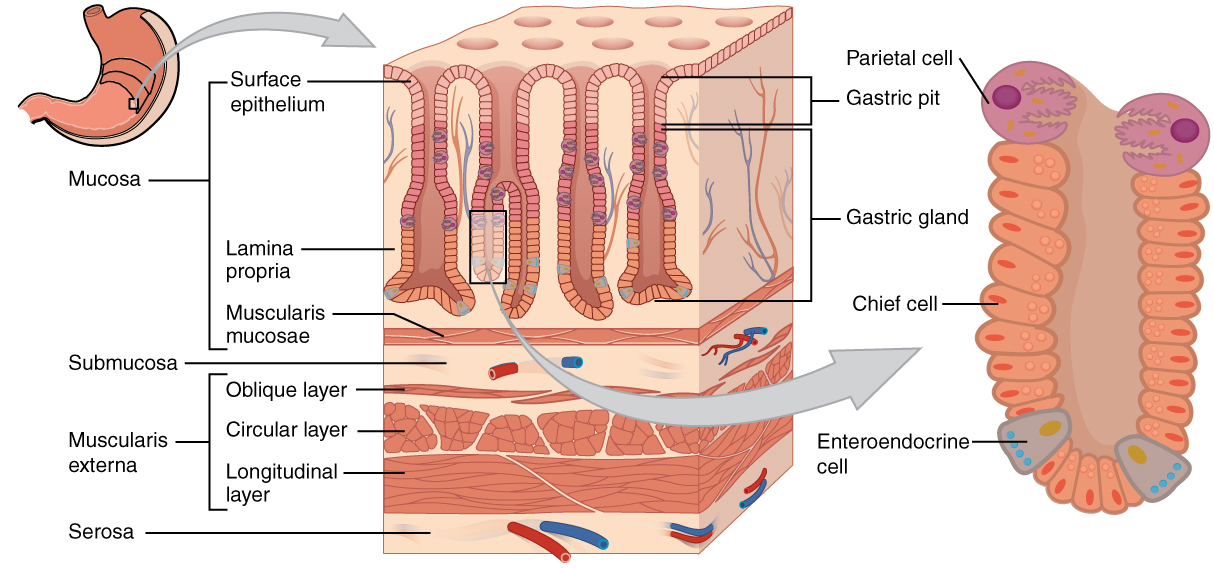
- Mucosa: The innermost layer containing gastric glands that produce acid and enzymes.
- Submucosa: A supportive layer rich in blood vessels, nerves, and connective tissue.
- Muscularis: Comprised of three muscle layers (longitudinal, circular, and oblique) that facilitate mechanical digestion.
- Serosa: The outermost protective layer.
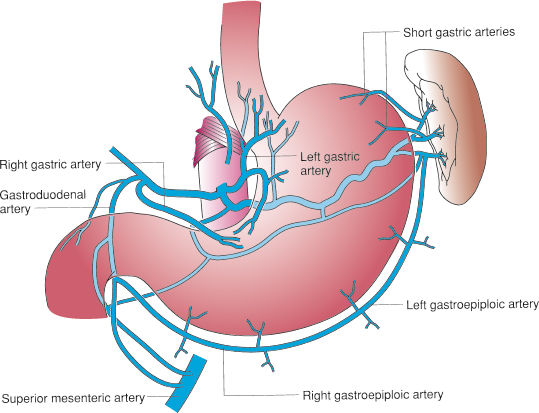
Gastric Blood Supply
- The stomach is mainly supplied by branches of the celiac trunk.
- Left and Right Gastric Arteries: Supply the lesser curvature of the stomach.
- Right and Left Gastroepiploic Arteries: Provide blood to the greater curvature.
- Short Gastric Arteries: Supply the fundus.
Physiology of the Stomach
-
Gastric Secretions:
- Hydrochloric Acid (HCl): Produced by parietal cells to lower pH for protein digestion and microbial defense.
- Pepsinogen: Secreted by chief cells and converted to pepsin to break down proteins.
- Mucus: Protects the stomach lining from acidic damage.
- Intrinsic Factor: Essential for vitamin B12 absorption in the small intestine.
- Gastrin: A hormone that stimulates acid secretion.
-
Mechanical Digestion:
- Muscular contractions mix and grind food, forming a semi-liquid substance known as chyme.
-
Regulation of Gastric Function:
- Neural Control: The enteric and autonomic nervous systems modulate secretions and motility.
- Hormonal Control: Hormones like gastrin, secretin, and cholecystokinin (CCK) coordinate digestive processes.
Gastric Disorders
-
Gastritis:
- Inflammation of the stomach lining, often due to infection, medication, or alcohol use.
-
Peptic Ulcers:
- Sores on the stomach or duodenal lining, commonly linked to H. pylori infection or NSAID use.
-
Gastro-Oesophageal Reflux Disease (GORD):
- A condition in which stomach acid frequently refluxes into the oesophagus, causing irritation.
-
Gastric Cancer:
- A malignancy of the stomach lining with risk factors such as H. pylori, smoking, and dietary influences.
Diagnosis and Treatment
-
Diagnostic Methods:
- Endoscopy: Direct visualization of the stomach lining and biopsy collection.
- Barium Swallow: Radiographic examination of the upper GI tract.
- Biopsy: Microscopic examination of tissue samples.
- Blood Tests: Evaluate for infections, anemia, and other markers.
-
Treatment Options:
- Medications: Antacids, proton pump inhibitors (PPIs), H2 receptor blockers, and antibiotics for H. pylori.
- Lifestyle Modifications: Dietary adjustments, weight management, and avoidance of triggers like alcohol and smoking.
- Surgical Interventions: Procedures such as gastrectomy for advanced ulcers or cancer.
Overview of Acid Secretion in the Stomach
Acid secretion is crucial for digestion. Hydrochloric acid (HCl) produced by parietal cells aids in food breakdown, enzyme activation, and protection against pathogens.
Mechanism of Acid Secretion
-
Parietal Cells:
- Located in the gastric glands primarily in the body and fundus, they secrete both HCl and intrinsic factor.
-
HCl Secretion Process:
- The H+,K+-ATPase (proton pump) exchanges intracellular hydrogen (H+) for extracellular potassium (K+).
- Chloride ions (Cl-) are transported into the lumen to form HCl.
- Bicarbonate generated within parietal cells is exchanged for chloride on the basolateral membrane, producing an alkaline tide after meals.
Regulation of Acid Secretion
-
Neural Regulation:
- Parasympathetic stimulation via the vagus nerve releases acetylcholine (ACh), which activates the proton pump on parietal cells.
-
Hormonal Regulation:
-
Gastrin:
- Secreted by G cells, it binds to CCK-B receptors on parietal cells to stimulate acid secretion.
-
Histamine:
- Released from enterochromaffin-like (ECL) cells, it enhances acid secretion via H₂ receptors.
-
Somatostatin:
- Produced by D cells, it inhibits acid secretion by suppressing gastrin and histamine release and directly acting on parietal cells.
-
Gastrin:
-
Local Factors:
- Prostaglandins (e.g., PGE₂) protect the gastric mucosa by inhibiting acid secretion and promoting mucus and bicarbonate production.
- Stomach distension and the presence of food also stimulate acid secretion through local reflexes.
Phases of Gastric Acid Secretion
-
Cephalic Phase:
- Triggered by sensory stimuli (sight, smell, taste, thought of food) and mediated by the vagus nerve, accounting for about 30% of acid secretion.
-
Gastric Phase:
- Initiated by the entry of food into the stomach (approximately 60% of secretion), stimulated by gastric distension and the presence of peptides.
-
Intestinal Phase:
- Occurs when chyme enters the small intestine, contributing about 10% to acid secretion and primarily acting as an inhibitory feedback mechanism.
Disorders Related to Acid Secretion
-
Gastro-Oesophageal Reflux Disease (GERD):
- Characterized by reflux of stomach acid into the oesophagus, leading to heartburn, regurgitation, and irritation.
-
Peptic Ulcer Disease:
- Results from the erosion of the stomach or duodenal lining due to excessive acid or reduced mucosal protection, often linked to H. pylori or NSAIDs.
-
Zollinger-Ellison Syndrome:
- A rare disorder featuring gastrin-secreting tumors that cause excessive acid production and recurrent ulcers.
Diagnosis and Treatment of Acid-Related Disorders
-
Diagnostic Methods:
- Endoscopy: For direct visualization and biopsy.
- pH Monitoring: To evaluate acid reflux in the oesophagus.
- Blood Tests: For detecting H. pylori and measuring gastrin levels.
-
Treatment Options:
- Medications: Antacids, PPIs, and H2 receptor blockers reduce acid production.
- Antibiotics: Used in combination with PPIs to eradicate H. pylori.
- Lifestyle Modifications: Dietary changes, weight management, and avoiding triggers.
- Surgical Interventions: For severe or refractory cases.
Final Summary
The stomach is integral to digestion through its combined mechanical and chemical processes. Its complex anatomy—with distinct regions, layers, and a robust blood supply—supports its function, while a sophisticated network of neural, hormonal, and local factors tightly regulates acid secretion. Understanding these processes is crucial for diagnosing and managing gastric disorders effectively.